Personal foot care
University Department of PodiatryWhat is personal foot care?
Personal foot care is part of a personal hygiene routine for feet and covers a set of tasks that an adult, whatever their age, would normally do for themselves if they are able to.
Toenail care |
|
Skin care |
|
Checking footwear |
|
How to carry out personal foot care
Personal foot care is important for everyone and can be carried out by yourself, a family member or carer to reduce pain, discomfort, improve confidence, quality of life and independence.
If you are diabetic and have been classed as low risk at your foot screening, these tips also apply to you, if you have been classed as moderate or high risk please seek professional advice.
Wash your feet often
- Wash and thoroughly dry your feet and change your socks every day
- Use mild soap, and wash between the toes
- But don’t soak them as this may destroy your skins natural oils
Dry your feet well
- Be sure to dry thoroughly, especially between the toes
- Fungal organisms love moisture, so depriving them of any wetness will make it more difficult to develop fungal infections
- When drying your feet, take a good look at the skin once a week on the bottom and top to looks for any changes in the skin
or nails
Filing skin
- Gently remove hard skin and calluses with a pumice stone or foot file when your skin is dry. Don’t overdo it or you could damage fresh skin underneath.
Moisturise
- If your skin is dry, apply moisturizing cream all over the foot, except for between the toes on a daily basis or more frequently if required
Cut toenails carefully
- Trim your toenails regularly using proper nail clippers. Cut straight across and avoid trimming too close to the skin or drastically rounding the corners of the nails, which can cause painful and cause ingrown toenails.
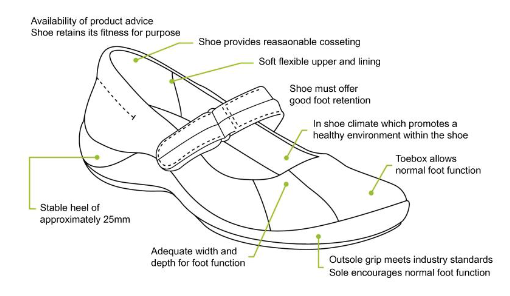
Shoes
- Always try your footwear on before buying a new pair, ideally in the afternoon as your feet swell throughout the day.
- Ensure your feet have been measured and you are wearing the correct size.
- Your footwear should always have laces/ straps/buckles to hold the shoe onto your foot and support you whilst walking, this will prevent any rubbing or friction and stop hard skin forming.
- Your shoe should be broad and rounded to accommodate your toes – avoid pointy shoes which can cramp your toes and cause ingrown toenails, callus and corns.
Footwear advice video
When and how to refer into NHS podiatry
| What we DON’T provide treatment for | What we DO provide treatment for * |
| Nail cutting | Foot ulceration |
| Fungal skin/ nails | Ingrown toenails (surgical removal) |
| Thickened nails | Musculoskeletal |
| Verrucae (not painful/less than 2 years) | Circulation assessments |
| Routine callus and corn reduction | Verrucae (painful and over 2 years) |
| Skin conditions e.g. athletes foot | Deep enucleation and electro surgery |
| Foot protection of high risk patients | |
| Painful lesions stopping you from walking |
*care plans and treatments will be carried out until improvement or resolution of foot complaint.
When a person does not meet the criteria for NHS podiatry care and has no family or carers in place, they can
seek personal care from a private podiatrist.
We recommend that when seeking private podiatry treatment that you ensure that the podiatrist is Health and Care Professions Councils (HCPC)
registered. Information can be found on the Health and Care Professions Councils website, to ensure they have the correct training to be safely and effectively carrying out your treatment.
Government advice
“Personal foot care includes the tasks that adults normally do for themselves such as cutting and filing toenails, smoothing and moisturising skin, looking for signs of infection or other problems which need referral to a podiatrist.”
Scottish Government Personal Foot Care Guidelines (2013).
If you would like further information please visit: Personal Foot Care Guidelines.
Useful Links
The personal foot care web page provides information and some short films about personal foot care.
Personal foot care – PDF booklet
Personal foot care – Looking after someone else’s feet – PDF booklet
Further information about personal foot care

W.A.S.P. is an acronym employed by our podiatrists to remind you of your current situation regarding your foot pain. It stands for Weight, Activity, Shoes and Partnership.
This is based on some of these areas of your lifestyle that go relatively unnoticed, in your life, until one day this comes sharply in to view then it stings you, resulting in your foot pain and now you pay attention, seeking help.
Weight reduction
People who tend to have increased weight can have more prolonged pain and poorer tissue healing due to increased levels of inflammation in the body. Reducing your weight can generally help improve and pain and the healing process.
Shoes
Shoes that have flexible soles generally offer the foot less support and can increase the stress in soft tissues in your feet. If you have shoelaces make sure they are tied appropriately. Avoid wearing hard, flat or unsupportive shoes.
Activity modification
Pacing is the term used for breaking down an activity or task. This can be done by taking regular breaks and prioritising daily activities can help. This can also help prevent ‘over-stimulating’ the pain system, so it is important to plan rests and set achievable goals.
Partnership
Your partnership with our MSK podiatrists, is based on the aims from NHS Scotland’s Realistic Medicine strategy, for you using healthcare services to feel empowered to discuss your treatment fully with our clinicians, including the possibility a suggested treatment might come with side effects – or even negative outcomes.
Additional information
Acute Injury Management
POLICE is an acronym (Protection, Optimal Loading, Ice, Compression and Elevation) that is used as a management strategy for many injuries and conditions for the first 24 to 72 hours.
- Protection and relative rest are advised immediately after injury for the first 24 to 72 hours.
- Optimal Loading refers to having a balanced rehabilitation program which encourages early and gradual activity to improve recovery. How you progress will vary from person to person depending on the injury. It is about finding the injured areas happy place and increasing slowly and gradually.
- Ice may be used for reducing pain and swelling. There are safety points to follow when you use ice:
- Don't ice over a numb area or open wound. If the skin is numb you won't notice if you're developing an ice burn and ice on an open wound can increase the risk of infection.
- Be wary of ice burns – don't apply ice directly to the skin, wrap an ice pack in a clean, damp tea towel before applying. Avoid prolonged exposure to ice, 10-20 minutes is usually adequate.
- Apply crushed ice/frozen peas wrapped in a damp towel for 10-20 minutes, 2-3 times per day for the first 5-7 days post injury/ flare up of pain.
- Stop applying ice if there are any negative effects such as increase in pain or swelling or skin soreness.
- Compression and Elevation are helpful for reducing inflammation. This can be done by keeping your joint raised on a pillow and compressed by wrapping a bandage around it.
Do not make the bandage too tight and do not wear tubi-grip or any compression bandage in bed at night. - Heat: After 2-3 days, you may find that heat is more relaxing.
You could use a heat pad or a hot water bottle with an insulated cover on it. Make sure this is not too hot and is not directly touching your skin.
You should do this for 10 to 15 minutes, 3 to 4 times a day.
What do I do if my symptoms flare up?
Flare ups of pain are common. Some people have recurrent flare ups of pain so it is important to know how best to manage these flare ups. In most cases a pain flare-up will settle within 6 weeks.
Top Tips
- You will likely find it helpful to rest a bit more but it is still important to keep active. This will help to avoid becoming stiff and your muscles becoming weak.
- If you aim to get a balance between rest and activity it should help your pain to settle down. You may be sore at first, however, start slowly and gradually increase the amount you do.
- Reduce movements or tasks that aggravate your symptoms. This can help especially in the early days.
- Adopting positions or movements that reduce your pain can be useful.
Pain Relief
Analgesia
- Analgesia also known as pain relief can be an important part in helping you manage your symptoms and allow you to stay active.
- Taking suitable pain relief regularly allows you to move more normally and continue your usual activities without causing any damage. It is unlikely that medication alone will resolve your pain totally. For this reason we are using the term pain relief (A 30-50% reduction in pain would be deemed to be a good success).
Paracetamol
- Paracetamol is a good general pain management medication. It is used to help manage lots of different types of pain.
- Sometimes people believe they need something ‘stronger’ than paracetamol when in fact, taking a regular dose rather than a one-off dose is more effective.
- Spreading the doses of the paracetamol evenly out over a day will help you control your pain. Visit NHS Inform for more detailed information on paracetamol.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
- NSAIDs are medications that can reduce swelling around joints and nerve endings to give pain relief. They are particularly useful
in treating inflammatory type pain. Two commonly prescribed NSAIDs are ibuprofen and naproxen. - Although NSAIDs can be very useful they are not suitable for everyone. Visit NHS inform for further information related to NSAIDs.
There are other forms of pain relievers available. If you feel your current pain relievers are not helping your pain or you are
experiencing any side effects from your medication, please seek advice from your GP or pharmacist.
For general information on medication visit NHS Inform.
Staying in work and returning to work
We know that staying in work or returning to work as soon as possible is good for your mental and physical health.
If you have problems with activities at work, it may be helpful to ask for a workstation/workplace assessment or talk with your manager or Occupational Health Department. This can help with alterations or provision of equipment or altering your working day or tasks.
There are organisations which can support you at work or help you return to work. You can visit Knowledge Scotland for further information.
Weight Management
Weight Reduction – People who are overweight tend to have more prolonged pain and poorer tissue healing due to increased levels of inflammation in the body. Reducing your weight can generally help improve the healing process.
A good indicator of whether you need to lose weight is your body mass index (BMI), which you can calculate with the NHS BMI calculator.
If your BMI states you are overweight or obese it is likely that losing weight will reduce your symptoms. Carrying extra fat also increases your risk of heart disease, stroke, type 2 diabetes, and some cancers. Reducing your portion sizes and eating a balanced diet can be helpful in reducing weight. NHS informs provides a free online 12-week weight management programme to get you started right away.
If you need a little more help and feel that you would benefit from working with others in group sessions NHS Lanarkshire’s Weigh to Go programme, groups in North and South Lanarkshire, will help you become more active, eat well and lead a healthier lifestyle.
Smoking
Smoking can affect how your body recovers from musculoskeletal problems. If you smoke then the good news is that by stopping smoking it can improve your health in many different ways. Giving up smoking is not something you have to do on your own. You’re twice as likely to stop smoking successfully if you get the right support from the NHS. There is a free NHS stop smoking service available in Lanarkshire to help you succeed.
Chronic Pain
Some people will have pain which persists beyond the expected time frame for their condition. For further information on this and how best to manage it please visit our Chronic Pain webpage.
Pain Association Scotland is a national charity that delivers professionally led self-management pain education in the community.
Active Health Programme
South Lanarkshire
Active Health is a programme for residents of South Lanarkshire living with long term conditions. Residents are referred via Acute, Physio & specialist nurses to a 10-week programme and then signposted onto a wide variety of mainstream physical activity, sport & outdoor opportunities.
South Lanarkshire Leisure and Culture have many active community opportunities as well as specialised referral programmes. Full details of the 20 leisure centres can be found on the SLL website. Contact details across South Lanarkshire or call 01698 476262 to find out the number of your local leisure centre.
Please contact your health professional to discuss this referral or contact SLLC on 01698 476262.
Contact details
- Phone Number: 01698 476 193
- Email: customer.services@southlanarkshireleisure.co.uk
- Address:
- South Lanarkshire Leisure & Culture HQ, First Floor
North Stand, Cadzow Avenue
Hamilton. ML3 0LX
- South Lanarkshire Leisure & Culture HQ, First Floor
-
Website: https://www.slleisureandculture.co.uk/info/34/health_and_fitness
North Lanarkshire
North Lanarkshire Leisure’s Active Health Programme in partnership with NHS Lanarkshire provides a range of supported programmes to help individuals realise the benefits of becoming more physically active whilst also assisting those who are recovering from minor or even more serious illness.
The Active Health Programme has both a General Programme where individuals can access the mainstream health and fitness programmes running within NL Leisure Venues including swimming, jogging, golf and more!
A Specialised Health Class Programme which requires a referral from a health professional, this option is available to individuals who require additional specialised support in taking part in physical activity and classes include Strength and Balance, Cardio I, Cardio II, Back Care and Macmillan Move More classes.
A health and social care professional can make a referral by using the Active Health referral form found at the bottom of the page in the link below.
Contact Details - Health & Wellbeing Information
- Telephone: 01236 341 709
- Email: melanie.menzies@nlleisure.com
- Website: https://www.nlleisure.co.uk/specialised-health-classes/active-health
Mental Wellbeing
It is very important to look after your own mental wellbeing. This can have an influence on your recovery or management of your Musculoskeletal problem. Visit our mental wellbeing page for more information.
If the advice on our website hasn't helped or improved your foot issue, you can self-refer and book an appointment.
Please complete our e-referral form and email this form to podiatry.hub@lanarkshire.scot.nhs.uk
The Podiatry Hub is open:
- Monday to Thursday - 8am-4pm
- Friday - 8am-3pm


NHS Lanarkshire Psychological Services: Digital Resources
Information for GPs and staff in all mental health services
Your Feedback – comments, concerns and complaints
NHS Lanarkshire is committed to improving the service it provides to patients and their families. We therefore want to hear from you about your experience. If you would like to tell us about this please visit our feedback page.

