Nail Conditions
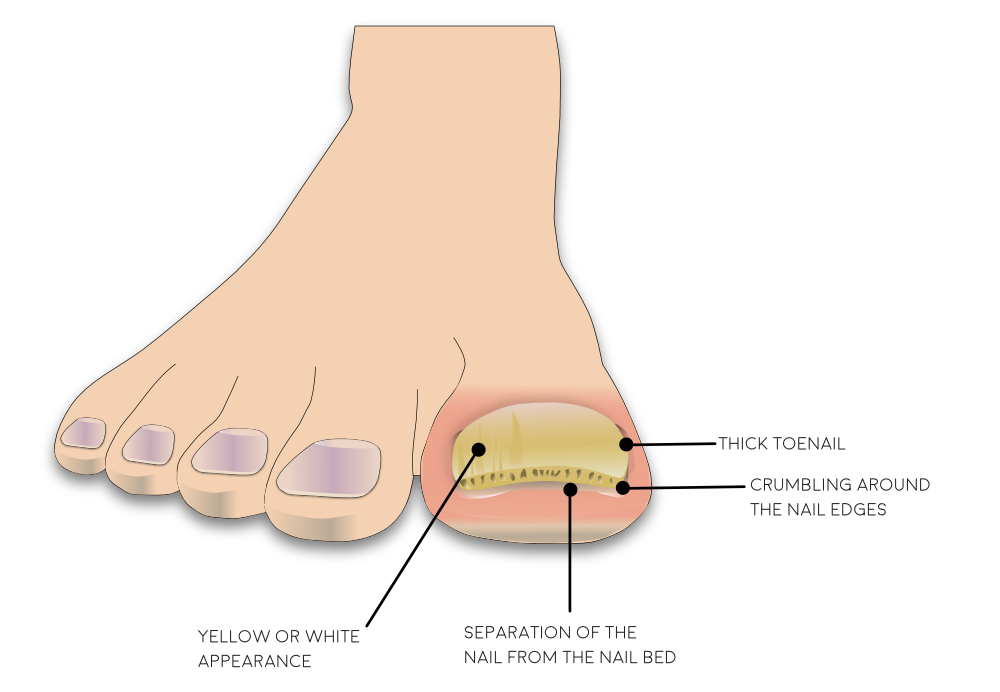
University Department of PodiatryThick Toenails
Thick nails, also known as onychauxis, is a nail disorder that could cause fingernails or toenails to grow abnormally thick.Over time, the nails may become curled and turn white or a yellow colour.
Symptoms may become more severe if left untreated. The nails may begin to curl and become too thick that it can be difficult to self-care.
Common Causes
The most common causes include:
- Fungal Infection
- Ill-fitting footwear
- Trauma
- Hereditary
- Health condition that effect the skin or nails e.g. Psoriasis
- Reduced circulation
- Diabetes
Thickened nails are not contagious and can’t be spread from person to person directly.
How to self care for thickened toenails
-
Treat underlying health conditions
Attend your GP if you think you may have a fungal infection or an underlying health condition that may be causing your thickened nails
-
Cut and file nails regularly
Regular cutting and filing of the nails will reduce the thickness and improve the appearance and any discomfort caused by the nail
-
Wear well-fitting shoes
Tight/narrow shoes can cause thick nails and can make symptoms worse- especially pain.
-
Move more
A boost in your circulation to your lower extremities (legs and feet) will increase the blood supply, oxygen and other nutrients may improve the unusual nail growth issue.
When to refer into NHS podiatry
If you cannot self-care or have a family member help, you may need to seek private podiatry care. Please ensure your practitioner is HCPC registered.
If you have regularly been self-managing your thickened nail and still have unmanageable pain or discomfort, you may choose to have nail surgery and have the nail permanently removed
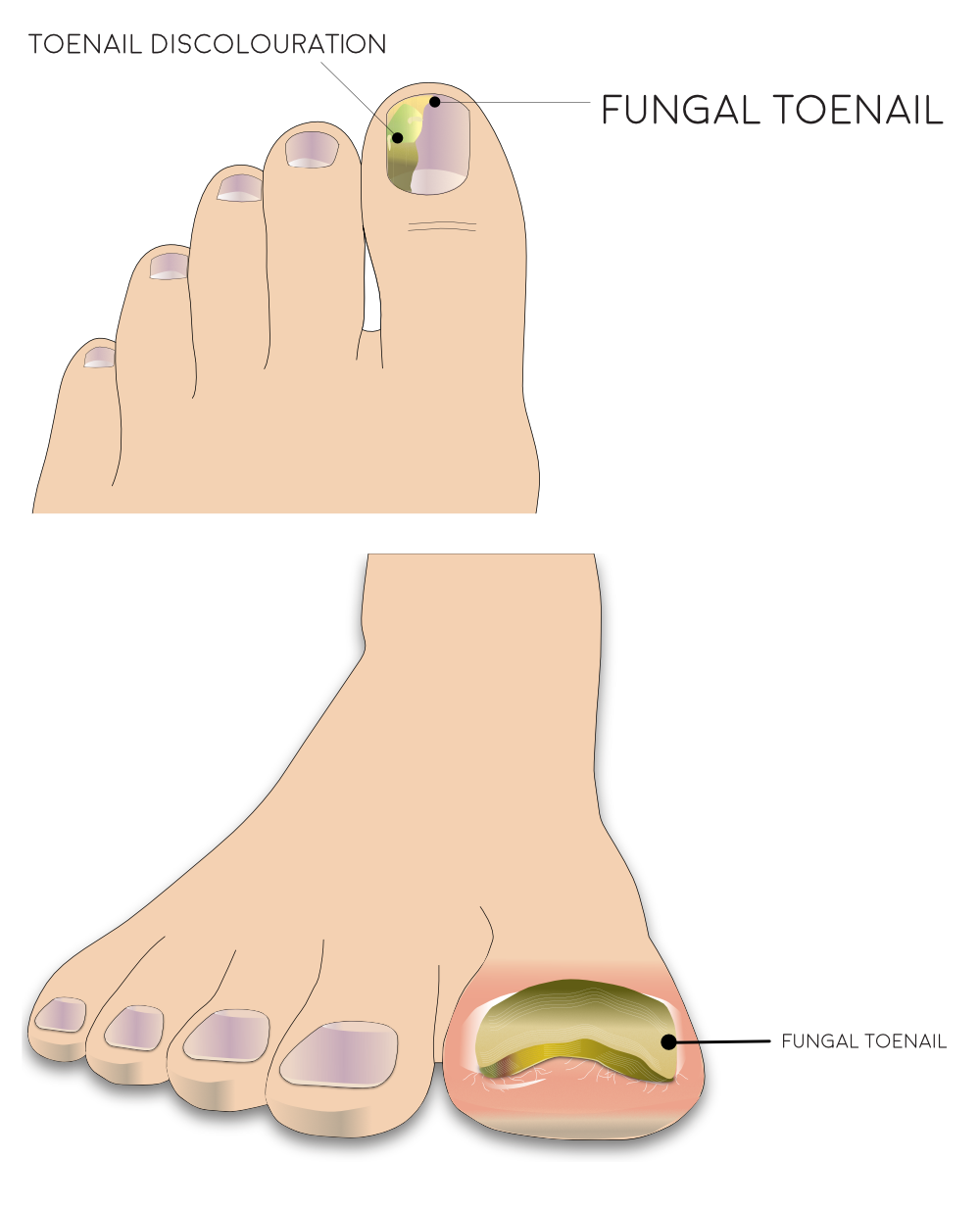
Fungal Toenails
A fungal nail infection (Onychomycosis) can affect any part of the nail. If left untreated and the infection worsens, the nail may become discoloured, change shape and the surrounding skin may thicken.
What are the signs and symptoms?
The nail may change in colour and shape. This can affect a single nail or several nails at one time. The first and fifth toenails are most commonly involved.
Different presentations include:
- Small flakey white patches and pits on the top of the nail plate.
- White or yellow streaks along one side of the nail.
- Debris may build up under the nail.
- The nail is discoloured and thickened
What can I do for fungal toenails?
-
Anti-fungal nail paints/Lacquer
You can purchase anti-fungal nail lacquers in your local pharmacy, health shops and supermarkets. File your nails weekly and apply a new coating of the lacquer as described on its packaging for up to 1 year.
-
Anti-fungal creams
You can purchase anti-fungal creams in your local pharmacy, health shops and supermarkets. Apply this to the infected nails and surrounding skin once a day. This can take up to 12 months to cure infection.
-
Oral tablet
If you are unsuccessful with the anti-fungal nail lacquer/ creams you may need to contact your GP for an oral anti-fungal treatment. You will be required to have a blood test prior to treatment to check your liver function and then take this medication .
How can I prevent fungal nail infections?
Do
- Keep your feet clean and dry
- Wear clean socks everyday
- Wear flip-flops in showers at the gym or pool
- Throw out old shoes
Don’t
- Wear shoes that make your feet hot and sweaty
- Share towels
- Wear other peoples shoes
- Share nail clippers/scissors
When to refer into NHS Podiatry
If you cannot self-care or have a family member help, you may need to seek private podiatry care.
Please ensure your practitioner is HCPC registered.
If your nails have thickened and cause pain/discomfort when walking or rub against the other toes you may require to have the nail permanently removed under local anaesthetic by your podiatrist.
Involuted (Curved) Toenails
A nail that grows in curved or curly at the sides is called an involuted nail. This can be painful as the nail can dig into the skin and may lead to an ingrown toenail.

What causes an involuted toenail?
- A major trauma
- Repeated pressure from shoes on long nails.
- Genetics
- Psoriasis, eczema and a number of other systematic diseases can affect the toenails.
How can I prevent an involuted toenail?
- Correctly trimming your nails. Cut them straight across and do not round the corners of the nail.
- Wear good fitting shoes with plenty of room at the toes.
- Try to avoid shoes with a small/shallow toe box such as pointed shoes.
When to refer into NHS Podiatry?
If you cannot self-care or have a family member help, you may need to seek private podiatry care.
We recommend that when seeking private podiatry treatment that you ensure that the podiatrist is Health and Care Professions Councils (HCPC)
registered. Information can be found on the Health and Care Professions Councils website, to ensure they have the correct training to be safely and effectively carrying out your treatment.
If self-care has not improved your symptoms and you are still having pain or infection suspected you may need to have the nail permanently removed under local anaesthetic by your podiatrist.
How can I self-care for an involuted toenail?
- Correctly trimming your nails. Cut them straight across and do not round the corners of the nail.
- Wear good fitting shoes with plenty of room at the toes.
- Try to avoid shoes with a small/shallow toe box such as pointed shoes.
Ingrown Toenails
An ingrown toenail, also known as onychocryptosis, is where a piece of nail cuts into the flesh of the toe. It can be extremely painful, red and swollen and in some cases it can cause pus and bleeding.
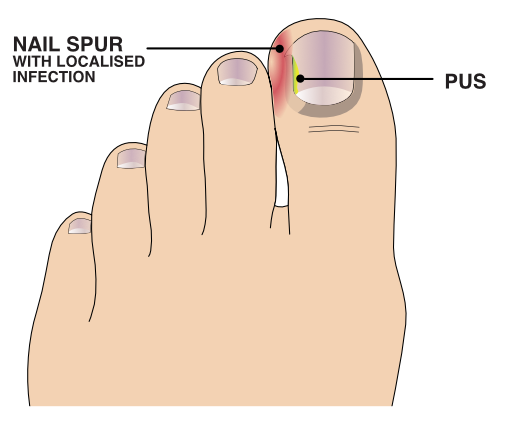
What causes an ingrown toenail?
- Cutting nails too short.
- Cutting the corners of the nail where it meets the skin.
- Picking toenails.
- Tight or ill-fitting shoes or hosiery.
- Excessive moisture.
- Damage/trauma to the nail or toe.
- Fungal infection.
- Naturally curved nails.
How can I prevent getting an ingrown toenail?
Do |
Don’t |
| Use the right equipment (eg. Nail nippers) and technique when cutting your nails. | Cut your nails to short. Ensure the nail is not lower than the edge of the skin. |
| Wear cotton socks as these are breathable. | Pick your toenails. |
| Change socks regularly throughout the day to prevent increased moisture. | Wear tight fitting shoes or shoes that are very narrow at the toes. |
| Ensure footwear and hosiery fit appropriately. |
How to self-care for an ingrown toenail
If left untreated, an ingrown toenail can become infected.
So it’s important that you:
- Keep your feet clean by washing them regularly with soap and water or salt water footbaths.
- Change your socks daily.
- Cut your toenails straight across, DO NOT cut down the side of your nail as this can worsen the condition.
- If you have picked your nail or cut it too short, allow it to grow out.
- Gently push the skin away from the nail using a cotton bud – you can try this after using a small amount of olive oil to soften the skin.
- Wear comfortable shoes that fit properly.
When to refer into NHS Podiatry?
- You will be seen by NHS Podiatry if you:
- Have an infection or your GP has prescribed antibiotics for an infection
- Have any underlying medical conditions (eg. Diabetes or taking immunosuppressant medication)
- Have tried to self-treat and had no improvement.
- Have seeked professional help and still had no improvement.
If this is your first episode of an ingrown toenail, the podiatrist may be able to resolve it by removing the spike.
Nail surgery may be recommended if your toenail doesn’t improve. Depending on the severity of your symptoms, this may involve permanently removing part or all of your toenail.
Further information about Nail Conditions
W.A.S.P. is an acronym employed by our podiatrists to remind you of your current situation regarding your foot pain. It stands for Weight, Activity, Shoes and Partnership.
This is based on some of these areas of your lifestyle that go relatively unnoticed, in your life, until one day this comes sharply in to view then it stings you, resulting in your foot pain and now you pay attention, seeking help.
Weight reduction
People who tend to have increased weight can have more prolonged pain and poorer tissue healing due to increased levels of inflammation in the body. Reducing your weight can generally help improve and pain and the healing process.
Shoes
Shoes that have flexible soles generally offer the foot less support and can increase the stress in soft tissues in your feet. If you have shoelaces make sure they are tied appropriately. Avoid wearing hard, flat or unsupportive shoes.
Activity modification
Pacing is the term used for breaking down an activity or task. This can be done by taking regular breaks and prioritising daily activities can help. This can also help prevent ‘over-stimulating’ the pain system, so it is important to plan rests and set achievable goals.
Partnership
Your partnership with our MSK podiatrists, is based on the aims from NHS Scotland’s Realistic Medicine strategy, for you using healthcare services to feel empowered to discuss your treatment fully with our clinicians, including the possibility a suggested treatment might come with side effects – or even negative outcomes.
Additional information
Acute Injury Management
POLICE is an acronym (Protection, Optimal Loading, Ice, Compression and Elevation) that is used as a management strategy for many injuries and conditions for the first 24 to 72 hours.
- Protection and relative rest are advised immediately after injury for the first 24 to 72 hours.
- Optimal Loading refers to having a balanced rehabilitation program which encourages early and gradual activity to improve recovery. How you progress will vary from person to person depending on the injury. It is about finding the injured areas happy place and increasing slowly and gradually.
- Ice may be used for reducing pain and swelling. There are safety points to follow when you use ice:
- Don't ice over a numb area or open wound. If the skin is numb you won't notice if you're developing an ice burn and ice on an open wound can increase the risk of infection.
- Be wary of ice burns – don't apply ice directly to the skin, wrap an ice pack in a clean, damp tea towel before applying. Avoid prolonged exposure to ice, 10-20 minutes is usually adequate.
- Apply crushed ice/frozen peas wrapped in a damp towel for 10-20 minutes, 2-3 times per day for the first 5-7 days post injury/ flare up of pain.
- Stop applying ice if there are any negative effects such as increase in pain or swelling or skin soreness.
- Compression and Elevation are helpful for reducing inflammation. This can be done by keeping your joint raised on a pillow and compressed by wrapping a bandage around it.
Do not make the bandage too tight and do not wear tubi-grip or any compression bandage in bed at night. - Heat: After 2-3 days, you may find that heat is more relaxing.
You could use a heat pad or a hot water bottle with an insulated cover on it. Make sure this is not too hot and is not directly touching your skin.
You should do this for 10 to 15 minutes, 3 to 4 times a day.
What do I do if my symptoms flare up?
Flare ups of pain are common. Some people have recurrent flare ups of pain so it is important to know how best to manage these flare ups. In most cases a pain flare-up will settle within 6 weeks.
Top Tips
- You will likely find it helpful to rest a bit more but it is still important to keep active. This will help to avoid becoming stiff and your muscles becoming weak.
- If you aim to get a balance between rest and activity it should help your pain to settle down. You may be sore at first, however, start slowly and gradually increase the amount you do.
- Reduce movements or tasks that aggravate your symptoms. This can help especially in the early days.
- Adopting positions or movements that reduce your pain can be useful.
Pain Relief
Analgesia
- Analgesia also known as pain relief can be an important part in helping you manage your symptoms and allow you to stay active.
- Taking suitable pain relief regularly allows you to move more normally and continue your usual activities without causing any damage. It is unlikely that medication alone will resolve your pain totally. For this reason we are using the term pain relief (A 30-50% reduction in pain would be deemed to be a good success).
Paracetamol
- Paracetamol is a good general pain management medication. It is used to help manage lots of different types of pain.
- Sometimes people believe they need something ‘stronger’ than paracetamol when in fact, taking a regular dose rather than a one-off dose is more effective.
- Spreading the doses of the paracetamol evenly out over a day will help you control your pain. Visit NHS Inform for more detailed information on paracetamol.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
- NSAIDs are medications that can reduce swelling around joints and nerve endings to give pain relief. They are particularly useful
in treating inflammatory type pain. Two commonly prescribed NSAIDs are ibuprofen and naproxen. - Although NSAIDs can be very useful they are not suitable for everyone. Visit NHS inform for further information related to NSAIDs.
There are other forms of pain relievers available. If you feel your current pain relievers are not helping your pain or you are
experiencing any side effects from your medication, please seek advice from your GP or pharmacist.
For general information on medication visit NHS Inform.
Staying in work and returning to work
We know that staying in work or returning to work as soon as possible is good for your mental and physical health.
If you have problems with activities at work, it may be helpful to ask for a workstation/workplace assessment or talk with your manager or Occupational Health Department. This can help with alterations or provision of equipment or altering your working day or tasks.
There are organisations which can support you at work or help you return to work. You can visit Knowledge Scotland for further information.
Weight Management
Weight Reduction – People who are overweight tend to have more prolonged pain and poorer tissue healing due to increased levels of inflammation in the body. Reducing your weight can generally help improve the healing process.
A good indicator of whether you need to lose weight is your body mass index (BMI), which you can calculate with the NHS BMI calculator.
If your BMI states you are overweight or obese it is likely that losing weight will reduce your symptoms. Carrying extra fat also increases your risk of heart disease, stroke, type 2 diabetes, and some cancers. Reducing your portion sizes and eating a balanced diet can be helpful in reducing weight. NHS informs provides a free online 12-week weight management programme to get you started right away.
If you need a little more help and feel that you would benefit from working with others in group sessions NHS Lanarkshire’s Weigh to Go programme, groups in North and South Lanarkshire, will help you become more active, eat well and lead a healthier lifestyle.
Smoking
Smoking can affect how your body recovers from musculoskeletal problems. If you smoke then the good news is that by stopping smoking it can improve your health in many different ways. Giving up smoking is not something you have to do on your own. You’re twice as likely to stop smoking successfully if you get the right support from the NHS. There is a free NHS stop smoking service available in Lanarkshire to help you succeed.
Chronic Pain
Some people will have pain which persists beyond the expected time frame for their condition. For further information on this and how best to manage it please visit our Chronic Pain webpage.
Pain Association Scotland is a national charity that delivers professionally led self-management pain education in the community.
Active Health Programme
South Lanarkshire
Active Health is a programme for residents of South Lanarkshire living with long term conditions. Residents are referred via Acute, Physio & specialist nurses to a 10-week programme and then signposted onto a wide variety of mainstream physical activity, sport & outdoor opportunities.
South Lanarkshire Leisure and Culture have many active community opportunities as well as specialised referral programmes. Full details of the 20 leisure centres can be found on the SLL website. Contact details across South Lanarkshire or call 01698 476262 to find out the number of your local leisure centre.
Please contact your health professional to discuss this referral or contact SLLC on 01698 476262.
Contact details
- Phone Number: 01698 476 193
- Email: customer.services@southlanarkshireleisure.co.uk
- Address:
- South Lanarkshire Leisure & Culture HQ, First Floor
North Stand, Cadzow Avenue
Hamilton. ML3 0LX
- South Lanarkshire Leisure & Culture HQ, First Floor
-
Website: https://www.slleisureandculture.co.uk/info/34/health_and_fitness
North Lanarkshire
North Lanarkshire Leisure’s Active Health Programme in partnership with NHS Lanarkshire provides a range of supported programmes to help individuals realise the benefits of becoming more physically active whilst also assisting those who are recovering from minor or even more serious illness.
The Active Health Programme has both a General Programme where individuals can access the mainstream health and fitness programmes running within NL Leisure Venues including swimming, jogging, golf and more!
A Specialised Health Class Programme which requires a referral from a health professional, this option is available to individuals who require additional specialised support in taking part in physical activity and classes include Strength and Balance, Cardio I, Cardio II, Back Care and Macmillan Move More classes.
A health and social care professional can make a referral by using the Active Health referral form found at the bottom of the page in the link below.
Contact Details - Health & Wellbeing Information
- Telephone: 01236 341 709
- Email: melanie.menzies@nlleisure.com
- Website: https://www.nlleisure.co.uk/specialised-health-classes/active-health
Mental Wellbeing
It is very important to look after your own mental wellbeing. This can have an influence on your recovery or management of your Musculoskeletal problem. Visit our mental wellbeing page for more information.
If the advice on our website hasn't helped or improved your foot issue, you can self-refer and book an appointment.
Please complete our e-referral form and email this form to podiatry.hub@lanarkshire.scot.nhs.uk
The Podiatry Hub is open:
- Monday to Thursday - 8am-4pm
- Friday - 8am-3pm


NHS Lanarkshire Psychological Services: Digital Resources
Information for GPs and staff in all mental health services
Your Feedback – comments, concerns and complaints
NHS Lanarkshire is committed to improving the service it provides to patients and their families. We therefore want to hear from you about your experience. If you would like to tell us about this please visit our feedback page.

