Metatarsalgia (Ball of the foot pain)
University Department of PodiatryOn this page
- What is Metatarsalgia?
- What are the common conditions that cause ball of the foot pain?
- Fat Pad Atrophy
- Capsulitis
- Intermetatarsal Bursitis
- Plantar Plate injury
- What Are The Symptoms Of Metatarsalgia (Ball of the foot pain)?
- What Causes It?
- What Can Help With Metatarsalgia (Ball of the foot pain)?
- Shoes
- Padding
- Pain Activity Ladder
- Exercise
- Printable Version
- Weight, Activity, Shoes, Partnership (W.A.S.P)
- Additional Information
What is Metatarsalgia (Ball of the foot pain)?
Metatarsalgia or ball of the foot pain is very common and will affect around 80% of the population at some point in their life. It is made up of a group of conditions that can cause pain and inflammation around the bones and joints in the ball of the foot. Finding comfortable footwear can be difficult.
Treatment protocols for ball-of-the-foot pain almost always start with basic principles and we would encourage you to consider trying some self-help treatment before making a referral to your local Podiatry department.
What are the common conditions that cause ball-of-the-foot pain?
The most common conditions affecting the ball of the foot are:
- Fatpadatrophy
- Capsulitis
- Intermetatarsal bursitis
- Plantar plate injury
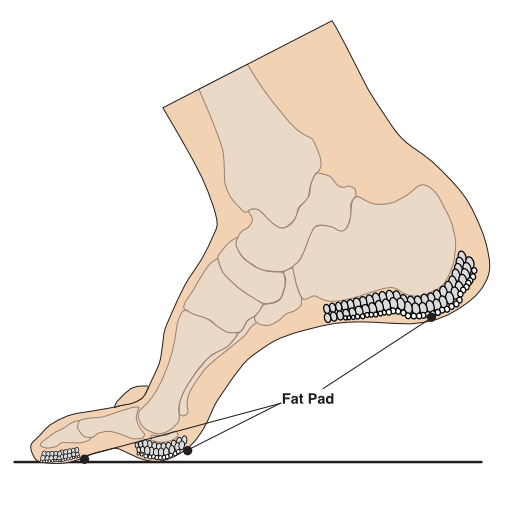
Fat pad atrophy
Fat pad atrophy is a term used to describe thinning and degeneration of the fat pad that sits under the ball of your foot. The fat pad is the soft tissue layer in between the skin and the bones. It has a honeycombed structure with fibro-elastic chambers containing fat globules which helps with shock absorption and the spreading of pressure across the ball of your foot during activity.
Thinning of the fat pad can lead to reduced shock absorption, making the foot more vulnerable to repetitive micro-trauma and developing inflammation, bruising, swelling and pain.
Thinning of the fat pad is a natural process and begins around the age of 30. It can take several years before the fat pad becomes thin enough to cause pain to develop. Fat pad atrophy is more common in people with Diabetes.
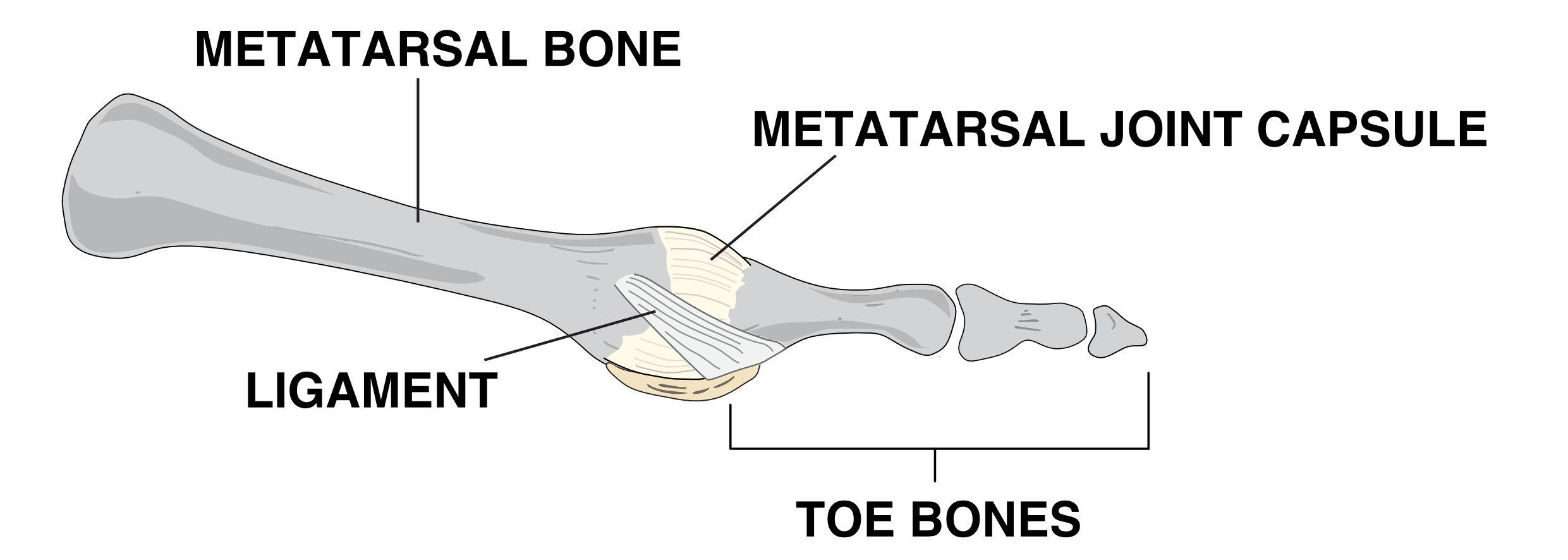
Capsulitis
Capsulitis is a term used to describe inflammation of a joint capsule.
A joint capsule is a covering that surrounds a joint and consists of a thick outer layer which gives it its strength and a thinner synovial layer which produces the fluid to lubricate the joint. Micro trauma or damage to the joint capsule can result in excess fluid being produced which causes the joint to swell and become painful when weight bearing. In your foot it most commonly affects the joint next to the big toe but can affect any joint within the body.
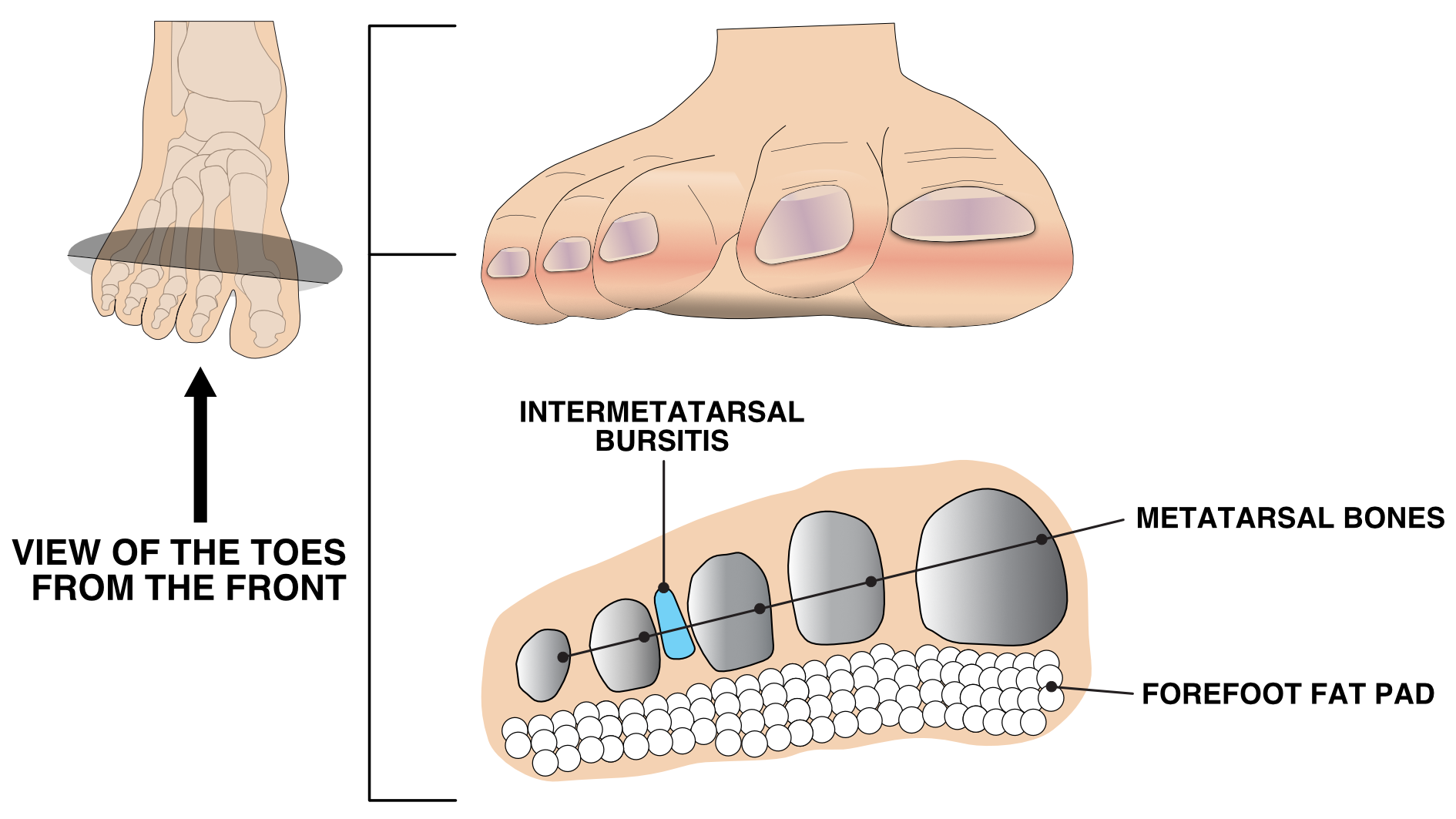
Intermetatarsal bursitis
Intermetatarsal bursitis is an inflammation of one of the bursa that is between the joints in the ball of the foot.
A bursa is a small sac of fluid that can help to increase shock absorption and reduce friction, its position within the ball of the foot is important as it helps prevent the bones from rubbing together.
When the bursa becomes inflamed it can swell and become painful when weight bearing. Tight fitting shoes can increase the compression of the bursa resulting in pain.
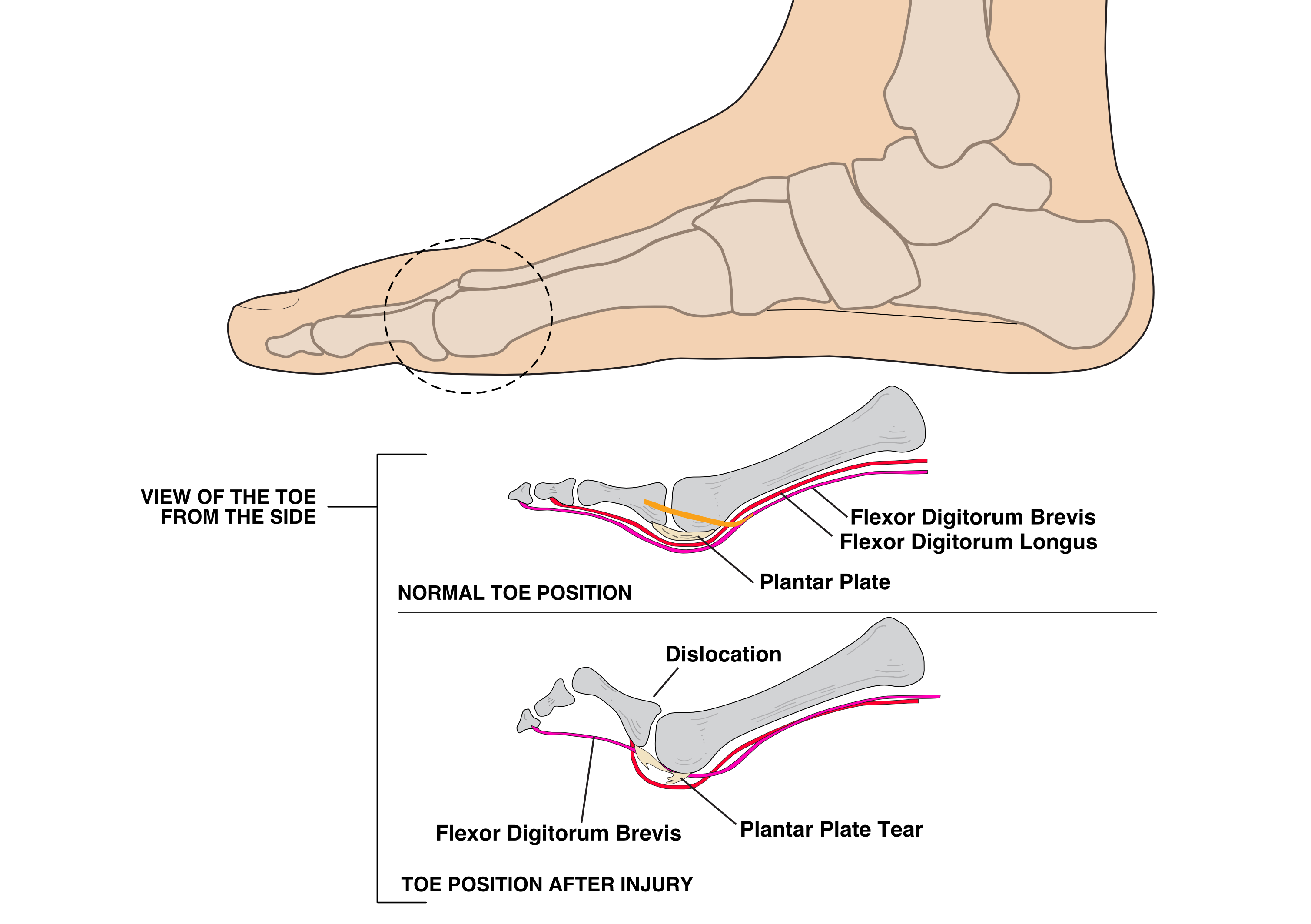
Plantar plate injury
The plantar plates are deep ligaments that form the bottom part of the joint capsule within each of the joints in the ball of the foot. The plantar plates help to stabilize the foot and toes when weight bearing and also provide the attachment of the plantar fascia into the base of the toes.
Repeated micro trauma can lead to tearing or partial tearing of the plantar plate. If left untreated this can cause deformity of the affected toe.
What are the signs and symptoms of Metatarsalgia (Ball of the foot pain)?
You may experience any or all of the following:
- A sharp, stabbing, burning or tingling sensation affecting the ball of the foot and into the toes
- Pain that increases with weight bearing activity and improves with rest
- Sensation of walking on a `pebble’ or `lump’
- Increased pain when walking barefoot, especially on a hard surface. The most common cause of pain in the ball of the foot is from a sudden increase in pressure or activity resulting in micro trauma and inflammation.
What causes metatarsalgia (Ball of the foot pain)?
You may have contributing factor related to metatarsalgia (ball of the foot pain):
- Being over-weight
- Age – the fat pad under the ball of the foot becomes thinner and this can increase pressure at the front of the foot.
- Increased swelling in feet
- High arched feet
- Tightness in the muscles in the back of the leg
- Weakness within the muscles in your foot/leg
- Unsuitable footwear that is too narrow or has a thin sole i.e. High heeled shoe
- Foot deformities such as hallux valgus (bunion), hallux limitus and hammer toe deformities
- Inflammatory conditions i.e. rheumatoid arthritis, psoriatic arthritis etc.
- Previous foot trauma i.e. metatarsal fracture, nerve injury
- Spending long periods standing, walking or running, especially with a sudden increase in these activities
What can help with Metatarsalgia (Ball of the foot pain)?
Unfortunately there is no quick or easy fix and your symptoms won’t improve overnight. It is important though that if you have any of the contributing factors you make the necessary changes to help with your recovery.
The advice below is aimed at reducing the pressure and inflammation from around the affected joints with a main focus on footwear and decreasing any tightness in the calf muscles. Tight calf muscles can increase the pressures through your forefoot (the front part of your foot). Your pain should improve but may take time to get better.
Making changes to your lifestyle as well as reducing aggravating activities is key to helping your recovery. Only you can do this.
There are a number of things you can try including:
- Rest and raise your foot on a stool when you can
- Put an ice pack (or bag of frozen peas) in a towel on the painful area for up to 20 minutes every 2 to 3 hours
- Wear shoes with cushioned heels and good arch support
- Use insoles in your footwear
- Try regular stretching and foot exercises
- Try exercises which put no pressure on your feet, such as swimming
- Try to lose weight if you’re overweight or obese
These a number of things to try to avoid including:
- Avoid walking or standing for long periods
- Avoid wearing high heels and tight pointy shoes
- Avoid wearing flip-flops or backless slippers
- Avoid walking barefoot on hard surfaces
Shoes
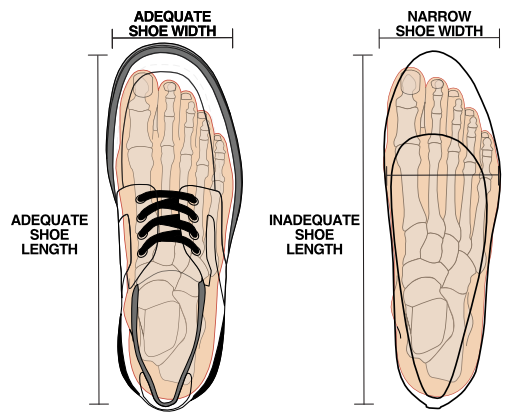
With ball of the foot pain it is important to make sure that your footwear fits well and are not too tight across the fore foot. Narrow footwear will increase compression through the joints and increase your pain. Shoes with a deep and wide toe box are preferable.
Footwear advice video
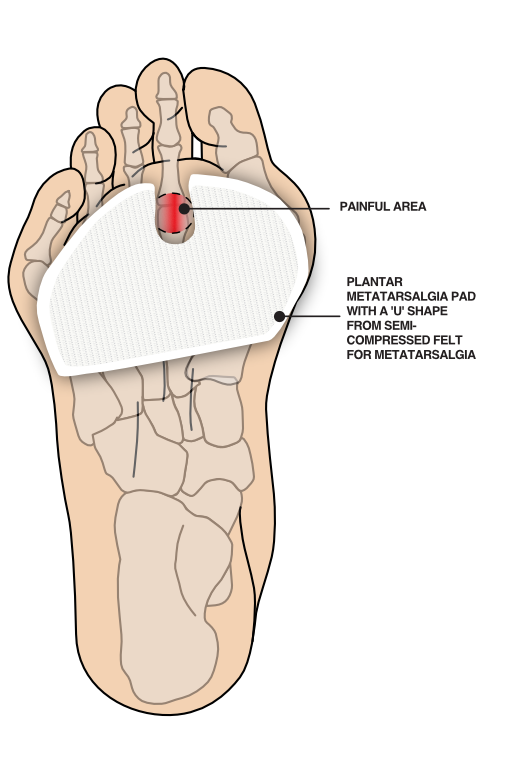
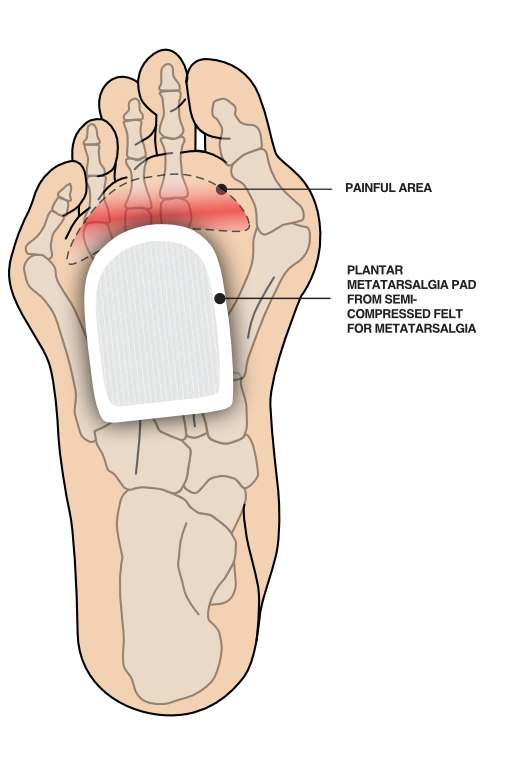
Padding
Padding can be applied to the bottom of the foot or on an insole, to help cushion and reduce the pressure on the joints. Padding comes in a variety of materials and can be bought from your local pharmacy or online.
Pain Activity Ladder
By following the pain activity ladder you can identify activities that you would consider severely painful, moderately painful and mildly irritating and act to change your habits.
The pain scale, most often used in healthcare, measures pain from 0-10 (zero being no pain and 10 representing the worst pain you could imagine).
If you can identify the level of pain you are experiencing, you will find out if you are in the green, amber or red zone. The best way to move down to the green zone is by pacing and spacing your activity.
When you are completing your rehabilitation exercises it is often best to work within the green (and sometimes amber zones depending on what you deem is an acceptable level of pain) both during the exercises and within 48 hours of completing your exercises. If you find yourself in the red zone you are likely pushing yourself too hard and may flare up the pain.
Ankle, Foot and Toe Exercise
The following exercises will help to improve your pain over a period of time. Remember to follow the advice from the Pain Activity Ladder section above.
- Video 1: Towel stretch
- Video 2: Intrinsic towel strengthening
- Video 3: Standing calf stretch
- Video 4: Intrinsic foot exercise using sports resistance band
- Video 5: Foot arch exercise using sports therapy ball
- Video 6: Toe motion exercises
Further information about Metatarsalgia (Ball of the foot pain)
W.A.S.P. is an acronym employed by our podiatrists to remind you of your current situation regarding your foot pain. It stands for Weight, Activity, Shoes and Partnership.
This is based on some of these areas of your lifestyle that go relatively unnoticed, in your life, until one day this comes sharply in to view then it stings you, resulting in your foot pain and now you pay attention, seeking help.
Weight reduction
People who tend to have increased weight can have more prolonged pain and poorer tissue healing due to increased levels of inflammation in the body. Reducing your weight can generally help improve and pain and the healing process.
Shoes
Shoes that have flexible soles generally offer the foot less support and can increase the stress in soft tissues in your feet. If you have shoelaces make sure they are tied appropriately. Avoid wearing hard, flat or unsupportive shoes.
Activity modification
Pacing is the term used for breaking down an activity or task. This can be done by taking regular breaks and prioritising daily activities can help. This can also help prevent ‘over-stimulating’ the pain system, so it is important to plan rests and set achievable goals.
Partnership
Your partnership with our MSK podiatrists, is based on the aims from NHS Scotland’s Realistic Medicine strategy, for you using healthcare services to feel empowered to discuss your treatment fully with our clinicians, including the possibility a suggested treatment might come with side effects – or even negative outcomes.
Additional information
Acute Injury Management
POLICE is an acronym (Protection, Optimal Loading, Ice, Compression and Elevation) that is used as a management strategy for many injuries and conditions for the first 24 to 72 hours.
- Protection and relative rest are advised immediately after injury for the first 24 to 72 hours.
- Optimal Loading refers to having a balanced rehabilitation program which encourages early and gradual activity to improve recovery. How you progress will vary from person to person depending on the injury. It is about finding the injured areas happy place and increasing slowly and gradually.
- Ice may be used for reducing pain and swelling. There are safety points to follow when you use ice:
- Don't ice over a numb area or open wound. If the skin is numb you won't notice if you're developing an ice burn and ice on an open wound can increase the risk of infection.
- Be wary of ice burns – don't apply ice directly to the skin, wrap an ice pack in a clean, damp tea towel before applying. Avoid prolonged exposure to ice, 10-20 minutes is usually adequate.
- Apply crushed ice/frozen peas wrapped in a damp towel for 10-20 minutes, 2-3 times per day for the first 5-7 days post injury/ flare up of pain.
- Stop applying ice if there are any negative effects such as increase in pain or swelling or skin soreness.
- Compression and Elevation are helpful for reducing inflammation. This can be done by keeping your joint raised on a pillow and compressed by wrapping a bandage around it.
Do not make the bandage too tight and do not wear tubi-grip or any compression bandage in bed at night. - Heat: After 2-3 days, you may find that heat is more relaxing.
You could use a heat pad or a hot water bottle with an insulated cover on it. Make sure this is not too hot and is not directly touching your skin.
You should do this for 10 to 15 minutes, 3 to 4 times a day.
What do I do if my symptoms flare up?
Flare ups of pain are common. Some people have recurrent flare ups of pain so it is important to know how best to manage these flare ups. In most cases a pain flare-up will settle within 6 weeks.
Top Tips
- You will likely find it helpful to rest a bit more but it is still important to keep active. This will help to avoid becoming stiff and your muscles becoming weak.
- If you aim to get a balance between rest and activity it should help your pain to settle down. You may be sore at first, however, start slowly and gradually increase the amount you do.
- Reduce movements or tasks that aggravate your symptoms. This can help especially in the early days.
- Adopting positions or movements that reduce your pain can be useful.
Pain Relief
Analgesia
- Analgesia also known as pain relief can be an important part in helping you manage your symptoms and allow you to stay active.
- Taking suitable pain relief regularly allows you to move more normally and continue your usual activities without causing any damage. It is unlikely that medication alone will resolve your pain totally. For this reason we are using the term pain relief (A 30-50% reduction in pain would be deemed to be a good success).
Paracetamol
- Paracetamol is a good general pain management medication. It is used to help manage lots of different types of pain.
- Sometimes people believe they need something ‘stronger’ than paracetamol when in fact, taking a regular dose rather than a one-off dose is more effective.
- Spreading the doses of the paracetamol evenly out over a day will help you control your pain. Visit NHS Inform for more detailed information on paracetamol.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
- NSAIDs are medications that can reduce swelling around joints and nerve endings to give pain relief. They are particularly useful
in treating inflammatory type pain. Two commonly prescribed NSAIDs are ibuprofen and naproxen. - Although NSAIDs can be very useful they are not suitable for everyone. Visit NHS inform for further information related to NSAIDs.
There are other forms of pain relievers available. If you feel your current pain relievers are not helping your pain or you are
experiencing any side effects from your medication, please seek advice from your GP or pharmacist.
For general information on medication visit NHS Inform.
Staying in work and returning to work
We know that staying in work or returning to work as soon as possible is good for your mental and physical health.
If you have problems with activities at work, it may be helpful to ask for a workstation/workplace assessment or talk with your manager or Occupational Health Department. This can help with alterations or provision of equipment or altering your working day or tasks.
There are organisations which can support you at work or help you return to work. You can visit Knowledge Scotland for further information.
Weight Management
Weight Reduction – People who are overweight tend to have more prolonged pain and poorer tissue healing due to increased levels of inflammation in the body. Reducing your weight can generally help improve the healing process.
A good indicator of whether you need to lose weight is your body mass index (BMI), which you can calculate with the NHS BMI calculator.
If your BMI states you are overweight or obese it is likely that losing weight will reduce your symptoms. Carrying extra fat also increases your risk of heart disease, stroke, type 2 diabetes, and some cancers. Reducing your portion sizes and eating a balanced diet can be helpful in reducing weight. NHS informs provides a free online 12-week weight management programme to get you started right away.
If you need a little more help and feel that you would benefit from working with others in group sessions NHS Lanarkshire’s Weigh to Go programme, groups in North and South Lanarkshire, will help you become more active, eat well and lead a healthier lifestyle.
Smoking
Smoking can affect how your body recovers from musculoskeletal problems. If you smoke then the good news is that by stopping smoking it can improve your health in many different ways. Giving up smoking is not something you have to do on your own. You’re twice as likely to stop smoking successfully if you get the right support from the NHS. There is a free NHS stop smoking service available in Lanarkshire to help you succeed.
Chronic Pain
Some people will have pain which persists beyond the expected time frame for their condition. For further information on this and how best to manage it please visit our Chronic Pain webpage.
Pain Association Scotland is a national charity that delivers professionally led self-management pain education in the community.
Active Health Programme
South Lanarkshire
Active Health is a programme for residents of South Lanarkshire living with long term conditions. Residents are referred via Acute, Physio & specialist nurses to a 10-week programme and then signposted onto a wide variety of mainstream physical activity, sport & outdoor opportunities.
South Lanarkshire Leisure and Culture have many active community opportunities as well as specialised referral programmes. Full details of the 20 leisure centres can be found on the SLL website. Contact details across South Lanarkshire or call 01698 476262 to find out the number of your local leisure centre.
Please contact your health professional to discuss this referral or contact SLLC on 01698 476262.
Contact details
- Phone Number: 01698 476 193
- Email: customer.services@southlanarkshireleisure.co.uk
- Address:
- South Lanarkshire Leisure & Culture HQ, First Floor
North Stand, Cadzow Avenue
Hamilton. ML3 0LX
- South Lanarkshire Leisure & Culture HQ, First Floor
-
Website: https://www.slleisureandculture.co.uk/info/34/health_and_fitness
North Lanarkshire
North Lanarkshire Leisure’s Active Health Programme in partnership with NHS Lanarkshire provides a range of supported programmes to help individuals realise the benefits of becoming more physically active whilst also assisting those who are recovering from minor or even more serious illness.
The Active Health Programme has both a General Programme where individuals can access the mainstream health and fitness programmes running within NL Leisure Venues including swimming, jogging, golf and more!
A Specialised Health Class Programme which requires a referral from a health professional, this option is available to individuals who require additional specialised support in taking part in physical activity and classes include Strength and Balance, Cardio I, Cardio II, Back Care and Macmillan Move More classes.
A health and social care professional can make a referral by using the Active Health referral form found at the bottom of the page in the link below.
Contact Details - Health & Wellbeing Information
- Telephone: 01236 341 709
- Email: melanie.menzies@nlleisure.com
- Website: https://www.nlleisure.co.uk/specialised-health-classes/active-health
Mental Wellbeing
It is very important to look after your own mental wellbeing. This can have an influence on your recovery or management of your Musculoskeletal problem. Visit our mental wellbeing page for more information.
If the advice on our website hasn't helped or improved your foot issue, you can self-refer and book an appointment.
Please complete our e-referral form and email this form to podiatry.hub@lanarkshire.scot.nhs.uk
The Podiatry Hub is open:
- Monday to Thursday - 8am-4pm
- Friday - 8am-3pm


NHS Lanarkshire Psychological Services: Digital Resources
Information for GPs and staff in all mental health services
Your Feedback – comments, concerns and complaints
NHS Lanarkshire is committed to improving the service it provides to patients and their families. We therefore want to hear from you about your experience. If you would like to tell us about this please visit our feedback page.

