Persistent Postural Perceptual Dizziness (PPPD or 3PD)
Persistent Postural Perceptual Dizziness
What is PPPD?
This is a sensation of constant vague dizziness or fog which has been present for more than three months and is usually worse on certain movements, or in busy places. Symptoms will usually improve if sitting in a quiet area or lying down, but not always.
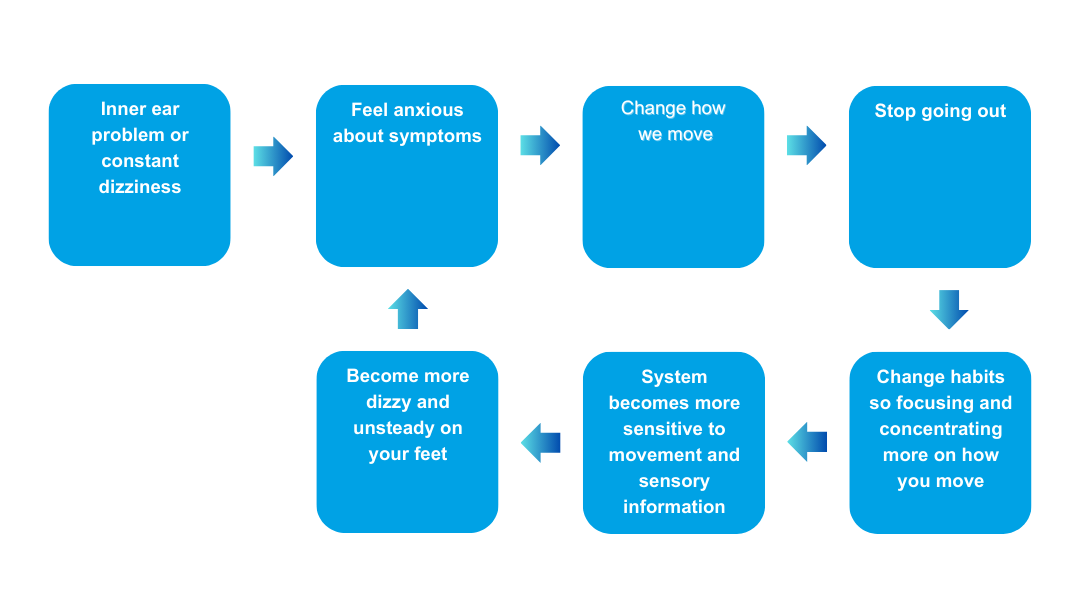
This usually occurs after an inner ear problem. Your brain adapts to help you cope with the dizzy feeling. This means you becomes more reliant on the eyes for balance and no longer move naturally. The inner ear stops interacting with the other parts of the balance system the way it had previously. As your eyes have more to do your brain struggles to keep you balanced which results in a lightheaded, or off balance sensation, which may cause you to stagger. In some cases this stays once the acute problem settles. When this happens we call that PPPD.
Often MRI and CT scans will be clear, this is because there is no structural damage to the brain. These tests are not used to diagnose PPPD as this occurs due to changes to how the brain uses the information.
What can be done to help this?
Your physiotherapist will create an exercise programme to help to address your individual triggers. The exercises will involve working up to your symptoms to allow your balance system to readjust to movement. They can be balance and walking exercises, focus exercises or watching videos to improve your tolerance of specific situations.
This will help your brain reprogram. As your balance system has become more sensitive it is important to do your exercises as instructed to ensure a smoother recovery. It will take time to carry over into your daily life as the tasks are broken down for the exercises and only when we are able to incorporate the exercises into life do we see the results. If your system is particularly adapted, then this may take several months to readjust.
Due to the nature of these symptoms it is common for people to feel anxious or stressed. If you are affected in this way your symptoms may feel worse and you may need some help to manage those feelings. Please discuss this with your therapist so we can look at ways of helping you manage the anxiety that can come with these sensations.
The NHSL has good information and courses to help us manage the stress and anxiety these symptoms can cause. Visit: Lanarkshire Mind Matters – https://www.lanarkshiremindmatters.scot.nhs.uk
It is common for people with PPPD to be referred to councilling and/or cognitive behavioural therapy (CBT). CBT and physiotherapy often gives the best results for this condition.
How long does it take for them to improve?
Each individual will respond differently, and your recovery will depend on the length of time you have been living with your symptoms, your confidence in returning to normal activity, any anxiety or fear associated these symptoms, age and your general activity level. In some cases, minor symptoms may remain.
Exercise
Once your balance improves, you should resume regular exercise which will help your balance system recover slowly. During your normal day to day activities and during exercise, you might think that keeping your head in a fixed position will help prevent dizziness but doing this actually does more harm than good. It is very important to move as naturally as possible to allow your balance system to return to normal.
Here are some simple balance exercises you could try at home:
- Practise standing with your feet closer together, try holding this position for 30 seconds. If you do not feel steady, try holding onto something. When you feel steady enough to do this without holding on then start doing this when you are washing your hands or brushing your teeth.
- Try walking outdoors each day even for 10-15 minutes, gradually building up time then adding in slopes or hills.
- When you reach into a cupboard try to look where you are reaching so you move your head more naturally.
Regular exercise is beneficial. To stay healthy, the UK Chief Medical Officers’ Physical Activity Guidelines, on GOV.UK, state that adults should try to be active every day and aim to do at least 150 minutes of physical activity over a week, through a variety of activities. This can be broken up to 40 minutes of exercise 3 x weekly or 15 minutes 3 x daily.
For more advice on your balance system and exercises see our balance page.
General Health
A good diet and healthy sleeping pattern will make you feel healthier. Reduce the amount of ‘screen time’ as this can cause eye strain. Alcohol can affect the part of the brain that controls balance so we advise reducing alcohol intake.
Make sure you have had a recent eye check with your optician. Eye strain can cause symptoms of dizziness.
Your GP may wish to monitor your blood pressure over a period of time. Both high and low blood pressure can cause dizziness. If you have palpitations, please inform your GP about this.
On occasions, dizziness can be brought on by prescription medication. This is especially so with:
- Antidepressants
- Epilepsy drugs
- Medications to control high blood pressure
- Anxiety medication
- Sleeping tablets
If you take one or a combination of these medications, it may be worthwhile speaking to your GP about the doses or whether or not you need them.
Medication
Your doctor and you may decide to use medication in your PPPD treatment. Note that usually medication alone does not fully address PPPD symptoms. Two types of antidepressants may be used.
- SSRIs (selective serotonin reuptake inhibitors), including fluvoxamine (Luvox®), paroxetine (Paxil®) and sertraline (Zoloft®)
- SNRIs (serotonin norepinephrine reuptake inhibitors), which are usually tried if two SSRIs have not worked
These medications are used to treat depression and anxiety, but they can also help to treat PPPD. All of them work in slightly different ways. If the first medication does not work or if it has too many side effects, your doctor may suggest trying a different one.
It is important to start at a low dose and increase the dose gradually. Let your doctor know if you are having any side effects. It usually takes 8 to 12 weeks for medication to start working. If you find a medication that helps with your symptoms, you may need to take it for several months. Do not stop taking your medication or change your dose without talking to your doctor.
Anti-vertigo and anti-sickness tablets can help during a bad attack of vertigo but we strongly discourage you from taking these medications on a regular basis especially for prolonged periods as they can cause side effects and prevent you from recovering from the original problem. Please do not take them to “prevent dizziness”. The evidence suggests that taking medications will slow down your recovery.
Mental Health
Sometimes, there will be some setbacks in your recovery. Many people with vertigo will feel anxious about resuming activities. This anxiety can affect your confidence in resuming physical activity and delay your recovery. Slow down and increase your activity slowly. Be reassured that feeling this way is quite natural and that most will make a good recovery.
Stress, low mood and anxiety can have many effects on the body. It can make vertigo worse. It is important to address this if you feel that this is a significant problem for you. Your GP may be able to advise you but there is useful online advice on these matters here:
Your Feedback – comments, concerns and complaints
NHS Lanarkshire is committed to improving the service it provides to patients and their families. We therefore want to hear from you about your experience. If you would like to tell us about this please visit our feedback page.

