Patellar Tendinopathy
On this page
- What Is Patellar Tendinopathy?
- What Are The Symptoms Of Patellar Tendinopathy?
- How Common Is Patellar Tendinopathy?
- What Causes Patellar Tendinopathy?
- What Can Help With Patellar Tendinopathy?
- Acute Injury Management
- Pacing And Spacing
- Exercise
- When to speak to a health professional
- Printable Version
Additional Information
- Pain Relief
- What do I do if my symptoms flare up?
- Mental Well Being
- Active Health Programme
- Staying in work and returning to work
- Smoking
- Chronic Pain
- Weight Management
Related pages
Patellar Tendinopathy
What Is Patellar Tendinopathy?
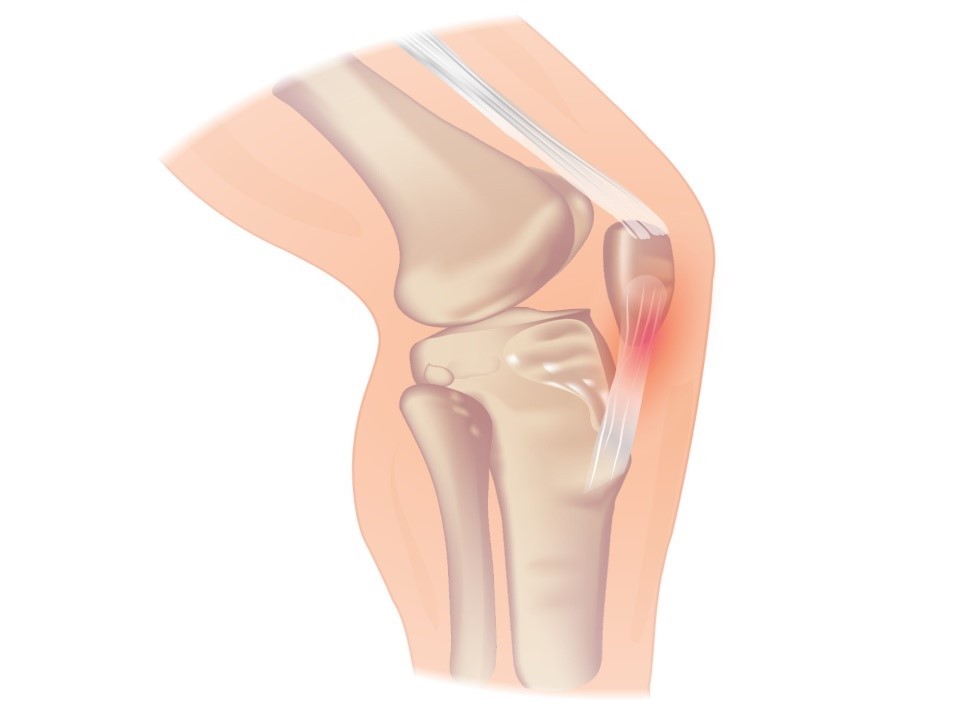
Patellar tendinopathy (Sometimes known as jumpers knee) is a common soft tissue injury which can cause pain in the tendon below the knee cap (patella). It can also cause stiffness and weakness around the knee.
The patellar tendon is important as it joins the thigh muscles (quadriceps) to the shin bone via the patella. The quadriceps are very important as they straighten the knee and are involved in functional everyday activities such as running, walking and going up and down stairs.
Patellar tendinopathy occurs when the patellar tendon is overused /overloaded.
The tendon struggles to cope with the pressure put upon it resulting in micro injuries and changes to its structure. This causes pain.
What Are The Symptoms Of Patellar Tendinopathy?
Symptoms normally appear gradually, but can also develop after a bump to the knee.
- Pain is the most common symptom, localised to the front of the knee (pain can be mild or severe).
- Tenderness on the front of the knee.
- The tendon can sometimes feel a little thickened. Some people can experience tightness or weakness in leg muscles (quadriceps).
- Stiffness in the knee can often occur– especially in the morning.
- Some people can also have mild swelling around the knee.
How Common Is Patellar Tendinopathy?
Patellar tendinopathy can affect anyone but is more common in the 15-30 years group. However, it is also common in older sporting individuals. It is normally more common in people who take part in jumping, running and hopping activities, such as football and tennis.
What Causes Patellar Tendinopathy?
It is not fully clear why some people develop patellar tendinopathy, but is normally due to several reasons:
- Repeated stress on the patellar tendon
- Overweight individuals
- A sudden increase in body weight
- Tightness of leg muscles
- Weakness in thigh muscles
- Changing activity levels or progressing too quickly
- Inappropriate footwear
- Exercising on hard surfaces
What Can Help With Patellar Tendinopathy?
Helpful Tips
Generally patellar tendon pain does not get better itself if you continue to put the tendon under too much stress. Patellar tendinopathy can resolve but this can take time. Physiotherapy exercises are recommended to strengthen the tendon. This will help improve the tendons “stress tolerance”.
It is advised that you check your daily activities. You may need to adapt your activity levels for your knee pain to settle. For example, you may need to reduce impact activities such as jumping.
However, it is recommended that you remain active. Low impact activities such as cycling and swimming will help you keep fit whilst you recover.
During physical activity, it is recommended that your pain is less than 3/10 and settles within a 24-hour period (See pain acitivity ladder).
By following this advice, you should be able to gradually increase your activity levels back to normal.
Other helpful tips
- Warm up before physical activity
- Regular leg stretching
- Ensure you take adequate rest during your weekly activities
- Don’t start new sport without some practice/ training first
Timescales/ Prognosis
An appropriate exercise programme can take more than 3 months to complete. You may see improvements before this but it may take longer for your symptoms to fully resolve.
Pacing And Spacing
- Pacing and spacing methods can help you manage your pain better.
- Pacing is the term used for breaking down an activity or task. This can be done by taking regular breaks. Prioritising daily activities can also help. This can prevent “over stimulating” your pain system.
- When completing challenging tasks or activities, it may be useful to set a “baseline”. This is the amount you can manage on a good or bad day without increasing your symptoms. Therefore you can plan rests and set achievable goals.
Pain Activity Ladder
- By following the pain activity ladder (Click here for a video explanation https://youtu.be/e9SEqd8bvII) which can be seen below, you can identify activities that you would consider severely painful, moderately painful and mildly irritating and act to change your habits.
- The pain scale, most often used in healthcare, measures pain from 0-10 (zero being no pain and 10 representing the worst pain you could imagine).
- If you can identify the level of pain you are experiencing, you will find out if you are in the green, amber or red zone. The best way to move down to the green zone is by pacing and spacing your activity.
- When you are completing your rehabilitation exercises it is often best to work within the green (and sometimes amber zones depending on what you deem is an acceptable level of pain) both during the exercises and within 48 hours of completing your exercises. If you find yourself in the red zone you are likely pushing yourself too hard and may flare up the pain.
Exercise
Along with managing your activity levels a graded exercise programme is the best way to help improve your pain and function for patellar tendinopathy. It is important to note it can take 6 – 12 weeks of doing specific exercises to notice a difference in your knee pain. Local NHS Lanarkshire physiotherapists have recorded exercise videos that will get your rehabilitation started and will guide you to manage your knee pain. The exercises are divided into early, middle and late stages. Your physiotherapist will help guide you. You should start doing the early exercises first and should find them easy before you progress to the middle exercises. Again you should begin to find the middle exercises easy before you progress to the later exercises. It is important to not overdo the exercises as this may irritate the tendon (See pain activity ladder).
When to speak to a health professional
If you find any of the above exercises worsen your symptoms, please stop and seek advice from a health professional.
Please seek immediate medical attention by phoning 111 if you experience knee trauma/injury with:
- A sudden pop/snap sensation
- Severe pain/swelling
- The inability to straighten your knee
If you experience swelling, redness with heat around your knee, please seek advice from your GP.
Help And Support
If after following the above advice, your symptoms have not improved within 6 to 12 weeks, a referral to a physiotherapist may be beneficial.
You can access physiotherapy by any of the following:
- Completing this online self-referral form
- Speak to your GP about a referral
When to speak to a health professional
If you find any of the above exercises worsen your symptoms, please stop and seek advice from a health professional.
Please seek immediate medical attention by phoning 111 if you experience knee trauma/injury with:
- a sudden pop/snap sensation
- severe pain/swelling
- the inability to straighten your knee
If you experience swelling, redness with heat around your knee, please seek advice from your GP.
Additional information
Acute Injury Management
POLICE is an acronym (Protection, Optimal Loading, Ice, Compression and Elevation) that is used as a management strategy for many injuries and conditions for the first 24 to 72 hours.
- Protection and relative rest are advised immediately after injury for the first 24 to 72 hours.
- Optimal Loading refers to having a balanced rehabilitation program which encourages early and gradual activity to improve recovery. How you progress will vary from person to person depending on the injury. It is about finding the injured areas happy place and increasing slowly and gradually.
- Ice may be used for reducing pain and swelling. There are safety points to follow when you use ice:
- Don't ice over a numb area or open wound. If the skin is numb you won't notice if you're developing an ice burn and ice on an open wound can increase the risk of infection.
- Be wary of ice burns – don't apply ice directly to the skin, wrap an ice pack in a clean, damp tea towel before applying. Avoid prolonged exposure to ice, 10-20 minutes is usually adequate.
- Apply crushed ice/frozen peas wrapped in a damp towel for 10-20 minutes, 2-3 times per day for the first 5-7 days post injury/ flare up of pain.
- Stop applying ice if there are any negative effects such as increase in pain or swelling or skin soreness.
- Compression and Elevation are helpful for reducing inflammation. This can be done by keeping your joint raised on a pillow and compressed by wrapping a bandage around it.
Do not make the bandage too tight and do not wear tubi-grip or any compression bandage in bed at night. - Heat: After 2-3 days, you may find that heat is more relaxing.
You could use a heat pad or a hot water bottle with an insulated cover on it. Make sure this is not too hot and is not directly touching your skin.
You should do this for 10 to 15 minutes, 3 to 4 times a day.
What do I do if my symptoms flare up?
Flare ups of pain are common. Some people have recurrent flare ups of pain so it is important to know how best to manage these flare ups. In most cases a pain flare-up will settle within 6 weeks.
Top Tips
- You will likely find it helpful to rest a bit more but it is still important to keep active. This will help to avoid becoming stiff and your muscles becoming weak.
- If you aim to get a balance between rest and activity it should help your pain to settle down. You may be sore at first, however, start slowly and gradually increase the amount you do.
- Reduce movements or tasks that aggravate your symptoms. This can help especially in the early days.
- Adopting positions or movements that reduce your pain can be useful.
Pain Relief
Analgesia
- Analgesia also known as pain relief can be an important part in helping you manage your symptoms and allow you to stay active.
- Taking suitable pain relief regularly allows you to move more normally and continue your usual activities without causing any damage. It is unlikely that medication alone will resolve your pain totally. For this reason we are using the term pain relief (A 30-50% reduction in pain would be deemed to be a good success).
Paracetamol
- Paracetamol is a good general pain management medication. It is used to help manage lots of different types of pain.
- Sometimes people believe they need something ‘stronger’ than paracetamol when in fact, taking a regular dose rather than a one-off dose is more effective.
- Spreading the doses of the paracetamol evenly out over a day will help you control your pain. Visit NHS Inform for more detailed information on paracetamol.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
- NSAIDs are medications that can reduce swelling around joints and nerve endings to give pain relief. They are particularly useful
in treating inflammatory type pain. Two commonly prescribed NSAIDs are ibuprofen and naproxen. - Although NSAIDs can be very useful they are not suitable for everyone. Visit NHS inform for further information related to NSAIDs.
There are other forms of pain relievers available. If you feel your current pain relievers are not helping your pain or you are
experiencing any side effects from your medication, please seek advice from your GP or pharmacist.
For general information on medication visit NHS Inform.
Staying in work and returning to work
We know that staying in work or returning to work as soon as possible is good for your mental and physical health.
If you have problems with activities at work, it may be helpful to ask for a workstation/workplace assessment or talk with your manager or Occupational Health Department. This can help with alterations or provision of equipment or altering your working day or tasks.
There are organisations which can support you at work or help you return to work. You can visit Knowledge Scotland for further information.
Weight Management
Weight Reduction – People who are overweight tend to have more prolonged pain and poorer tissue healing due to increased levels of inflammation in the body. Reducing your weight can generally help improve the healing process.
A good indicator of whether you need to lose weight is your body mass index (BMI), which you can calculate with the NHS BMI calculator.
If your BMI states you are overweight or obese it is likely that losing weight will reduce your symptoms. Carrying extra fat also increases your risk of heart disease, stroke, type 2 diabetes, and some cancers. Reducing your portion sizes and eating a balanced diet can be helpful in reducing weight. NHS informs provides a free online 12-week weight management programme to get you started right away.
If you need a little more help and feel that you would benefit from working with others in group sessions NHS Lanarkshire’s Weigh to Go programme, groups in North and South Lanarkshire, will help you become more active, eat well and lead a healthier lifestyle.
Smoking
Smoking can affect how your body recovers from musculoskeletal problems. If you smoke then the good news is that by stopping smoking it can improve your health in many different ways. Giving up smoking is not something you have to do on your own. You’re twice as likely to stop smoking successfully if you get the right support from the NHS. There is a free NHS stop smoking service available in Lanarkshire to help you succeed.
Chronic Pain
Some people will have pain which persists beyond the expected time frame for their condition. For further information on this and how best to manage it please visit our Chronic Pain webpage.
Pain Association Scotland is a national charity that delivers professionally led self-management pain education in the community.
Active Health Programme
South Lanarkshire
Active Health is a programme for residents of South Lanarkshire living with long term conditions. Residents are referred via Acute, Physio & specialist nurses to a 10-week programme and then signposted onto a wide variety of mainstream physical activity, sport & outdoor opportunities.
South Lanarkshire Leisure and Culture have many active community opportunities as well as specialised referral programmes. Full details of the 20 leisure centres can be found on the SLL website. Contact details across South Lanarkshire or call 01698 476262 to find out the number of your local leisure centre.
Please contact your health professional to discuss this referral or contact SLLC on 01698 476262.
Contact details
- Phone Number: 01698 476 193
- Email: customer.services@southlanarkshireleisure.co.uk
- Address:
- South Lanarkshire Leisure & Culture HQ, First Floor
North Stand, Cadzow Avenue
Hamilton. ML3 0LX
- South Lanarkshire Leisure & Culture HQ, First Floor
-
Website: https://www.slleisureandculture.co.uk/info/34/health_and_fitness
North Lanarkshire
North Lanarkshire Leisure’s Active Health Programme in partnership with NHS Lanarkshire provides a range of supported programmes to help individuals realise the benefits of becoming more physically active whilst also assisting those who are recovering from minor or even more serious illness.
The Active Health Programme has both a General Programme where individuals can access the mainstream health and fitness programmes running within NL Leisure Venues including swimming, jogging, golf and more!
A Specialised Health Class Programme which requires a referral from a health professional, this option is available to individuals who require additional specialised support in taking part in physical activity and classes include Strength and Balance, Cardio I, Cardio II, Back Care and Macmillan Move More classes.
A health and social care professional can make a referral by using the Active Health referral form found at the bottom of the page in the link below.
Contact Details - Health & Wellbeing Information
- Telephone: 01236 341 709
- Email: melanie.menzies@nlleisure.com
- Website: https://www.nlleisure.co.uk/specialised-health-classes/active-health
Mental Wellbeing
It is very important to look after your own mental wellbeing. This can have an influence on your recovery or management of your Musculoskeletal problem. Visit our mental wellbeing page for more information.
Your Feedback – comments, concerns and complaints
NHS Lanarkshire is committed to improving the service it provides to patients and their families. We therefore want to hear from you about your experience. If you would like to tell us about this please visit our feedback page.

