Frozen Shoulder
On this page
- What is a frozen shoulder?
- What are the symptoms of a frozen shoulder?
- How common is a frozen shoulder?
- What causes a frozen shoulder?
- Will it affect the other shoulder?
- What can help with a frozen shoulder?
- What are your other treatment options for a frozen shoulder?
- When to speak to a health professional
- Help and Support
- Printable Version
Additional Information
- Pain Relief
- What do I do if my symptoms flare up?
- Mental Well Being
- Active Health Programme
- Staying in work and returning to work
- Smoking
- Chronic Pain
- Weight Management
Related pages
Information about Frozen Shoulder
What is a frozen shoulder?
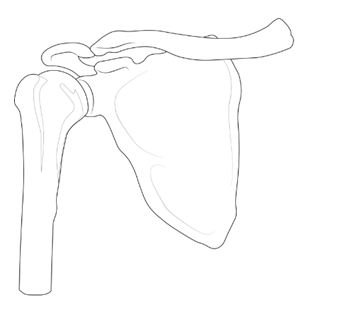
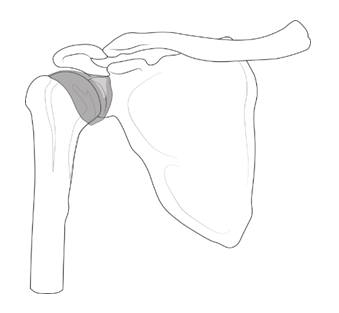
It is a condition which affects the lining that surrounds the shoulder joint, which is called the capsule. This becomes inflamed, which is painful and the shoulder also stiffens up.
Key points:
- A frozen shoulder is a painful stiff shoulder
- People often experience significant pain and very restricted movements; the pain can last for between two and nine months
- It can take anywhere between 12 and 42 months to fully resolve
- Most of the care is about pain control, accepting the limitations and waiting for it to get better
- Physiotherapy and shoulder injection can be helpful for some people
- Some people whose symptoms do not improve may need to have surgery
The capsule thickens over time which limits movement. When it does start to improve it tends to be a slow process but your shoulder may always have some movement restriction in the future. Although the pain usually gets better, it may never go away completely.
Shoulder Joint
Thickened shoulder capsule
What are the symptoms of a frozen shoulder?
- Pain in the shoulder and upper arm
- The pain can be severe and tends to be constant, which can interfere with your sleep
- Pain can be a lot worse on reaching for things or when lying on that side
- The shoulder may stiffen up quickly
- The restricted movement can stop you putting your hand behind you, or being able to reach as far as the back of your head
How common is a frozen shoulder?
- It is quite common in people aged 40-60 and more common in people who have diabetes or cardiovascular disease.
What causes a frozen shoulder?
- We don’t know. Sometimes a specific event will happen that results in a frozen shoulder, like an injury or a recent surgery. Most of the time there is no obvious cause.
Will it affect the other shoulder?
- About 10% of people can expect to experience symptoms in their other shoulder in the future. This risk is higher in people with diabetes.
What can help with a frozen shoulder?
No one treatment has been shown to cure a frozen shoulder and on average a frozen shoulder can last about two and a half years.
What can you do to control the symptoms?
The aims of treatment are:
- Pain relief
- Improving range of motion
- Reducing duration of symptoms
- Returning to normal activities
Shoulders are designed to move and inactivity is harmful to the tissues around the joint. With a frozen shoulder pain doesn’t equal damage therefore maintaining movement within the limits of your pain is important. However, you may want to avoid doing tasks that aggravate your pain too often. Adjusting how you do certain tasks can help manage your pain, for example, putting your sore arm in first to a jumper or jacket and taking it out last.
More Advice on solutions to help you with activities of daily living can be found here:
- North Lanarkshire: makinglifeeasier.org.uk
- South Lanarkshire: http://www.careinfoscotland.scot/topics/care-at-home/equipment-and-adaptionstelecare/
Exercise
The following exercises can help with improving movement and function of your shoulder and arm.
- VIDEO 1: Early pendulum shoulder movement
- VIDEO 2: Early shoulder movement
- VIDEO 3: Early shoulder movement
- VIDEO 4: Middle shoulder movement
- VIDEO 5: Middle shoulder movement
- VIDEO 6: Late shoulder movement
- VIDEO 7: Late shoulder movement

What are your other treatment options for a frozen shoulder?
Corticosteroid injection – Steroid injections into the joint (+/- local anaesthetic) may be offered. It can be difficult to predict how much this might help and any relief they give is generally short term.
The physiotherapist will advise you on when to re-start the exercises after you receive the steroid injection. A second injection may be required in a small number of cases.
Injections may not be suitable for every person.
Distension arthrogram or hydrodilatation – These are similar procedures and involve injecting a volume of fluid into the shoulder joint to stretch the capsule. Not all people are suitable for these procedures, and these treatment options are not always available in all hospitals. The results are variable and not everyone gets significant improvement from them.
Manipulation under anaesthesia (MUA) – This involves direct physical manipulation of the shoulder under general anaesthetic to hopefully improve the movement.
Surgery – An arthroscopic (keyhole) capsular release uses a camera in the joint to guide the release (cutting) of some of the thickened capsule. Surgery is not a reliable way to make the frozen shoulder go away but can sometimes help. If the pain associated with frozen shoulder remains severe for a long time, surgery may be discussed as an option.
What are the risks of surgery?
Risks include infection, nerve injury, bleeding and fracture of the humerus bone. A general anaesthetic is usually fairly low risk. However, if you have significant general health problems, the risks with the anaesthetic go up significantly and it may not be sensible to do surgery due to risks of stroke, heart attack and blood clots.
When to speak to a health professional
It is important to seek medical help in certain situations:
- If you are in extreme levels of pain
- If you have had a traumatic incident such as a fall, which results in you being unable to move your arm at all
- If you have any pins and needles or numbness in your arm
- If the skin over your shoulder is hot, red or swollen
- If you feel feverish, unwell or have unusual levels of tiredness
- If you have been experiencing unexplained weight loss or night-time sweating
Help And Support
If after following the above advice, your symptoms have not improved within 6 to 12 weeks, a referral to a physiotherapist may be beneficial.
You can access physiotherapy by any of the following:
- Completing this online self-referral form
- Speak to your GP about a referral
What do I do if my symptoms flare up?
Flare ups of pain are common. Some people have recurrent flare ups of pain so it is important to know how best to manage these flare ups. In most cases a pain flare-up will settle within 6 weeks.
Top Tips
- You will likely find it helpful to rest a bit more but it is still important to keep active. This will help to avoid becoming stiff and your muscles becoming weak.
- If you aim to get a balance between rest and activity it should help your pain to settle down. You may be sore at first, however, start slowly and gradually increase the amount you do.
- Reduce movements or tasks that aggravate your symptoms. This can help especially in the early days.
- Adopting positions or movements that reduce your pain can be useful.
Pain Relief
Analgesia
- Analgesia also known as pain relief can be an important part in helping you manage your symptoms and allow you to stay active.
- Taking suitable pain relief regularly allows you to move more normally and continue your usual activities without causing any damage. It is unlikely that medication alone will resolve your pain totally. For this reason we are using the term pain relief (A 30-50% reduction in pain would be deemed to be a good success).
Paracetamol
- Paracetamol is a good general pain management medication. It is used to help manage lots of different types of pain.
- Sometimes people believe they need something ‘stronger’ than paracetamol when in fact, taking a regular dose rather than a one-off dose is more effective.
- Spreading the doses of the paracetamol evenly out over a day will help you control your pain. Visit NHS Inform for more detailed information on paracetamol.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
- NSAIDs are medications that can reduce swelling around joints and nerve endings to give pain relief. They are particularly useful in treating inflammatory type pain. Two commonly prescribed NSAIDs are ibuprofen and naproxen.
- Visit NHS Inform for further information related to NSAIDS
There are other forms of pain relievers available. If you feel your current pain relievers are not helping your pain or you are experiencing any side effects from your medication, please seek advice from your GP or pharmacist.
For general information on medication visit NHS Inform.
Staying in work and returning to work
We know that staying in work or returning to work as soon as possible is good for your mental and physical health.
If you have problems with activities at work, it may be helpful to ask for a workstation/workplace assessment or talk with your manager or Occupational Health Department. This can help with alterations or provision of equipment or altering your working day or tasks.
There are organisations which can support you at work or help you return to work. You can ask your physiotherapist or Occupational Therapist for information or visit Knowledge Scotland.
Weight Management
Weight Reduction – People who are overweight tend to have more prolonged pain and poorer tissue healing due to increased levels of inflammation in the body. Reducing your weight can generally help improve the healing process.
A good indicator of whether you need to lose weight is your body mass index (BMI), which you can calculate with the NHS BMI calculator.
If your BMI states you are overweight or obese it is likely that losing weight will reduce your symptoms. Carrying extra fat also increases your risk of heart disease, stroke, type 2 diabetes, and some cancers. Reducing your portion sizes and eating a balanced diet can be helpful in reducing weight. NHS informs provides a free online 12-week weight management programme to get you started right away.
If you need a little more help and feel that you would benefit from working with others in group sessions NHS Lanarkshire’s Weigh to Go programme, groups in North and South Lanarkshire, will help you become more active, eat well and lead a healthier lifestyle.
Smoking
Smoking can affect how your body recovers from musculoskeletal problems. If you smoke then the good news is that by stopping smoking it can improve your health in many different ways. Giving up smoking is not something you have to do on your own. You’re twice as likely to stop smoking successfully if you get the right support from the NHS. There is a free NHS stop smoking service available in Lanarkshire to help you succeed.
Chronic Pain
Some people will have pain which persists beyond the expected time frame for their condition. For further information on this and how best to manage it please visit our Chronic Pain webpage.
Pain Association Scotland is a national charity that delivers professionally led self-management pain education in the community.
Active Health Programme
South Lanarkshire
Active Health is a programme for residents of South Lanarkshire living with long term conditions. Residents are referred via Acute, Physio & specialist nurses to a 10-week programme and then signposted onto a wide variety of mainstream physical activity, sport & outdoor opportunities.
South Lanarkshire Leisure and Culture have many active community opportunities as well as specialised referral programmes. Full details of the 20 leisure centres can be found on the SLL website. Contact details across South Lanarkshire or call 01698 476262 to find out the number of your local leisure centre.
Please contact your health professional to discuss this referral or contact SLLC on 01698 476262.
Contact details
- Phone Number: 01698 476 193
- Email: customer.services@southlanarkshireleisure.co.uk
- Address:
- South Lanarkshire Leisure & Culture HQ, First Floor
North Stand, Cadzow Avenue
Hamilton. ML3 0LX
- South Lanarkshire Leisure & Culture HQ, First Floor
-
Website: https://www.slleisureandculture.co.uk/info/34/health_and_fitness
North Lanarkshire
North Lanarkshire Leisure’s Active Health Programme in partnership with NHS Lanarkshire provides a range of supported programmes to help individuals realise the benefits of becoming more physically active whilst also assisting those who are recovering from minor or even more serious illness.
The Active Health Programme has both a General Programme where individuals can access the mainstream health and fitness programmes running within NL Leisure Venues including swimming, jogging, golf and more!
A Specialised Health Class Programme which requires a referral from a health professional, this option is available to individuals who require additional specialised support in taking part in physical activity and classes include Strength and Balance, Cardio I, Cardio II, Back Care and Macmillan Move More classes.
A health and social care professional can make a referral by using the Active Health referral form found at the bottom of the page in the link below.
Contact Details – Health & Wellbeing Information
- Telephone: 01236 341 709
- Email: melanie.menzies@nlleisure.com
- Website: https://www.nlleisure.co.uk/specialised-health-classes/active-health
Mental Well Being
It is very important to look after your own mental wellbeing. This can have an influence on your recovery or management of your Musculoskeletal problem. Visit our mental wellbeing page for more information.
Your Feedback – comments, concerns and complaints
NHS Lanarkshire is committed to improving the service it provides to patients and their families. We therefore want to hear from you about your experience. If you would like to tell us about this please visit our feedback page.


