
Maternity Services
Being pregnant and giving birth is a unique experience. These pages have been developed to give you some information which you may find helpful during your pregnancy and baby’s birth.
Please use any information in conjunction with your ‘READY STEADY BABY BOOK’ and the information from your named midwife.
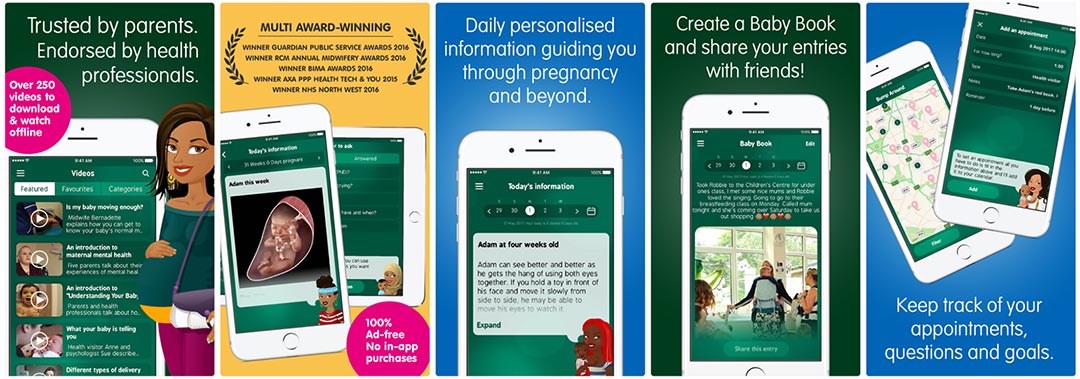
There are now mobile APPS available free to Smartphone users, so it is even easier for you and your partner to find out about pregnancy, birth and early parenting. We would strongly recommend Best Beginning’s Baby Buddy APP which as has been endorsed by the Royal Colleges of Obstetrics and Gynaecologists (RCOG) and Midwives (RCM).
Maternity Unit
The Maternity Unit at University Hospital Wishaw opened in June 2001 and provides a labour and birthing environment which takes into consideration your unique needs and preferences.
Maternity Inpatient Services – Walkthrough video
Images below show outside the maternity unit, a scan room, birthing room and birthing pool

Preconceptual care
Preconception health is the mental and physical health and wellbeing of men and women during their reproductive years, before and between pregnancies.
All men and women can benefit from good preconception health, whether or not they plan to have a baby now, or in the future.
Good preconception health is important for increasing your chances of getting pregnant (if or when you choose to) and having a healthy pregnancy.
Key messages for preconception health
-
Contraception and sexual health
Men and women should practice safer sex to avoid sexually transmitted infections and unintended pregnancy. If you are sexually active and do not want to become pregnant, there are a range of contraception methods available to you. Please see our Lanarkshire Sexual Health website for more information.
-
Mental health
Positive mental health and wellbeing is important for you and your baby. Find out more about mental health and wellbeing and the support services available on our elament website. If you take medication for a mental health problem, speak to your GP or other health professional before becoming pregnant.
-
Healthy weight
Eating well and achieving a healthy weight is important for fertility (in men and women) and healthy pregnancy and birth outcomes. You should aim to be a healthy weight, which means having a body mass index between 18.5 and 24.9 kg/m2. Visit the NHS Inform website for information on eating well in pregnancy.
-
Folic acid
Women who are planning a pregnancy, or who may become pregnant, should take a daily folic acid supplement of 400 micrograms, at least one month prior to pregnancy and for the first 12 weeks. This reduces the risk of neural tube defects. Healthy Start vitamins contain folic acid, vitamin C and vitamin D and are suitable for use before, during and after pregnancy. Some women are at higher risk of having a baby with a neural tube defect (e.g. those with a family history or those with a body mass index of 30 or more) and may be prescribed a daily folic acid supplement of 5 milligrams by their GP.
-
Alcohol
If you are planning a pregnancy or think you could become pregnant, the safest approach is not to drink alcohol at all, to keep risks to your baby to a minimum. Drinking in pregnancy can lead to long-term harm to your baby, with the more you drink the greater the risk. Men should avoid excessive drinking (as this can affect fertility) and if they choose to drink, drink within recommended limits. Further information about alcohol and support services can be found on NHS inform’s alcohol and pregnancy page.
-
Smoking
Men and women who are planning pregnancy or who may become pregnant should stop smoking as this can be harmful to you, your unborn baby and those around you. Our Quit Your Way service can help those who want to give up.
-
Drugs
No illegal drugs are safe for use in pregnancy or when planning pregnancy. For more information about drugs and the support services available, visit NHS inform’s taking drugs in pregnancy web page. If you are using illegal drugs and finding it difficult to stop, speak to your GP or health professional for help and access to contraception.
If you are planning pregnancy and take prescription drugs, discuss this with your GP to ensure these are safe to take during pregnancy.
-
Healthy relationships
Being in a healthy and happy relationship before pregnancy is best for you and any children you may have. If you have experienced any form of gender-based violence and would like support, visit NHS inform’s Violence and abuse in pregnancy page for advice.
-
Immunisation
If you are planning pregnancy or may become pregnant, you should check if you are protected against rubella. You are protected if you have had two doses of the MMR (mumps, measles and rubella) vaccine. If you are unsure, ask your GP to check your vaccine history. If you haven’t had two doses of MMR, ask to get the vaccination. MMR vaccine could cause risk to your baby in pregnancy so you should avoid becoming pregnant for one month after having it. Further information on immunisation is available on the NHS Inform website.
Related links
Early Pregnancy Assessment Unit
Ward open 9am-5pm, Monday to Friday.
Women can self- refer to our Early Pregnancy Service on 01698 366217 if they have had positive pregnancy test and experience abdominal pain or vaginal bleeding.
Women with a history of miscarriages who are pregnant again can contact us to discuss their care needs.
Our specialist team of staff may offer self-care advice, ask you to come to hospital to see a doctor, or offer an ultrasound scan appointment depending on your symptoms and pregnancy history but this may not be on the same day.
We follow National Guidelines for ultrasound scanning in early pregnancy.(NICE)
If you are well and less than 6 weeks pregnant we may ask you to self- care at home and repeat a pregnancy test in 1 week and call us back with the result to arrange follow up.
If you are more than 6 weeks pregnant with vaginal bleeding we may offer you an early ultrasound scan within 48 hours if you have a recent positive pregnancy test
If your symptoms change or worsen after speaking to us please call us back to discuss and plan your care needs again.
If you have had a private scan which needs hospital follow up, please call us to arrange the appropriate timing of a hospital scan. This this may mean waiting 7-14 days depending on your private scan findings-we will discuss this fully with you.
We also have an early pregnancy scan service at Hairmyres Hospital which you can self-refer to if you are well and this hospital is easier for you to access care. Early pregnancy at Hairmyres can be contacted on 01355 584501.
We may ask you to contact your GP if your symptoms are not pregnancy related.
Antenatal Care
Positive pregnancy test – ‘Keep Calm & Call the Midwife’
All women are offered an opportunity to book a first appointment with a midwife, who will help them plan their pregnancy care.
It is important you contact a midwife as early as possible after learning of the pregnancy.
Please contact your GP surgery and ask for an appointment with the midwife. The receptionist will help you arrange your first appointment.
**If you are not registered with a GP, then please attend your local healthcare Centre and ask the receptionist for contact details of your local midwife team**
Your first appointment lasts approximately 1 hour. You will meet your named midwife who will provide care within your local community healthcare facility. We will offer choices for your pregnancy which ensure you have a tailored package of care which meets your unique needs. For some women, this means care will be delivered by a team of healthcare providers to ensure the best outcome for woman and her baby.
The majority of inpatient services are based in the maternity at University Hospital Wishaw. We also have maternity day assessment units at Wishaw, Airdrie, East Kilbride and Lanark.
You will be given a booklet ‘your guide to screening tests during pregnancy 2016 edition’ to enable you to make a fully informed choice. Further information is available in the You’re pregnant! Scans and tests document.
Immunisation
Immunisation in pregnancy is important to ensure you and your baby receive protection. Further advice can be accessed from the following websites for:
- Recommended vaccines in pregnancy – https://www.nhsinform.scot/healthy-living/immunisation/when-to-immunise/pregnancy-and-baby/
- Influenza- info for pregnant women – https://www.nhsinform.scot/healthy-living/immunisation/vaccines/flu-vaccine/
- Whooping cough – https://www.nhsinform.scot/healthy-living/immunisation/vaccines/whooping-cough-vaccine/
- MMR – https://www.nhsinform.scot/healthy-living/immunisation/vaccines/mmr-vaccine/
Scanning
We will offer you an ultrasound scan to confirm how many weeks pregnant you are. If you are uncertain about having a scan, please tell the midwife who will be happy to discuss this with you. If you wish to have a scan, please drink 1 pint of fluid before your appointment (not milk). This helps to fill your bladder and makes it easier to get a clear picture of your baby.
Blood tests
It is important to emphasise that you do not have to provide blood samples or agree to all the tests we may offer you.
Preparation for Birth and Parenting
Being pregnant and becoming a parent are among the most important things that can happen to you. Giving birth is a major life event. You may want to learn more about your developing baby, changes in your body, how to keep healthy and also the birth itself.
When you discover you are pregnant, you want your baby to have the best start in life. It’s good to know what vitamins help your baby’s development in the womb, what are the best foods to eat; drinks to limit or avoid altogether. We can also offer advice/help on smoking and quitting for you, your partner and anyone else who lives with you. Ask your midwife about Healthy Start Vitamins.
We offer the following classes where both you and your birth partner are welcome to attend. Just ask your community midwife to help you book a session.
- Active Birth Sessions
- Refresher birth course
- Baby resuscitation classes
- Infant feeding workshop
- Breastfeeding support group
- Physiotherapy postnatal exercises
Ask your midwife about organsations based within your community that also give support to families:
Keeping active whether your pre or post natal can really make a difference to you and your baby’s health and wellbeing. North Lanarkshire Leisure has created an enjoyable range of sessions across their venues specifically tailored for you from yoga to aquafit to swimming and walking.
For more information check out classes on www.nlleisure.co.uk or email melanie.menzies@nlleisure.com
Other Contacts which may be useful:
- NHS 24 – 111 (from mobile and landline)
- Scottish Domestic Abuse Helpline 0800 027 1234 (24 hours)
- Motherwell & District Women’s Aid 01698 322020
- Money Matters app – download from your device’s store
- Lanarkshire Sexual Health & Well being: http://www.lanarkshiresexualhealth.org http://www.lansh.scot.nhs.uk
- Family planning clinics: http://www.lansh.scot.nhs.uk/adult-clinics
- C card: http://www.lansh.scot.nhs.uk/services/directory/c-card-centres
- Young person clinics: http://www.lansh.scot.nhs.uk/young-peoples-services
CrossReach Perinatal Services
Are you pregnant or have children under 2? Are you struggling with how you are feeling? You are not alone. Support is here for you.
E-mail: bluebell@crossreach.org.uk
Telephone: 0141 221 3003
For more information see our CrossReach Perinatal Services Leaflet
If pregnancy, labour or postnatal advice is needed
Please contact your Community Midwife or Team office between 8:45am and 4:45pm.
For emergency care including any concerns about your babies’ movements, please contact Maternity Triage – 01698 366210 open 24 hours.
Your birth plan
We want this to be a very special day for you, so please take time to write down a birth plan.
What matters to you, is very important so please hand this to your midwife when you present in labour. You can now upload you own personal birth plan onto your badger notes if you have access to these via your phone. There will be opportunity to discuss this during your community Midwife appointments.
Advice from Physiotherapist - ANTE-NATAL
Stay Active
Maintaining your health and fitness is just as important during your pregnancy as it is at any other time in your life.
For exercises and advice on how best to stay fit and healthy during your pregnancy please see the Pelvic Obstetric and Gynaecological Physiotherapy’s booklet below.
Common conditions during pregnancy
During the course of your pregnancy, many changes will occur in your body. This can sometimes cause aches in your muscles and joints which you have never previously experienced. These symptoms normally resolve following the delivery of your baby.
For advice on how best to manage these symptoms whilst pregnant, please see the Pelvic Obstetric and Gynaecological Physiotherapy’s booklet below.
Pelvic Floor Exercises
Hormonal and weight changes during pregnancy can place extra stress on the pelvic floor muscles. Make sure you exercise these muscles regularly to prevent any leakages.
Check out the video and/or the Pelvic Obstetric and Gynaecological Physiotherapy’s booklet below for further advice.
- https://www.youtube.com/watch?v=v731EXFR2k4
This video was produced by NHS Highland in conjunction with Association for Continence Advice - The Pelvic Floor Muscles – a Guide for Women booklet
If you are struggling with your exercises or any pelvic health issues seek help from your local GP, physiotherapist or nurse.
Relaxation
Relaxation is a technique you can use during your pregnancy and afterwards.
It can be used at any time to reduce muscle tension and can help you to rest more effectively. Relaxation is best performed in side lying after 19 weeks of pregnancy.
Read the Pelvic Obstetric and Gynaecological Physiotherapy’s booklet below:
Listen to the Mitchell Method of Relaxation below
Advice from Physiotherapist - Labour and Birthing
Have you made a birth plan?
Watch the video below for some hints and tips about breathing and the best positions for labour and delivery.
- Positions for Labour and Delivery video
This video was produced by NHS Greater Glasgow and Clyde
Caesarean Section

Enhanced Recovery for Obstetric Surgery in Scotland (EROSS) is a national patient-centred care pathway. The aim of EROSS is to improve patient recovery while ensuring a high standard of patient care. Have you elected for a C-Section?
Follow the links below to ensure your comfort in the early recovery period.
Video: EROSS – Physiotherapy advice for after your Caesarean Journey video
Booklet: My Caesarean Delivery Journey: the enhanced recovery approach
Advice from Physiotherapist - POST-NATAL
Recovery Advice
Fit for the Future
Following your pregnancy, it is important to ensure your body recovers and re-gains pre-pregnancy levels of health and fitness.
For exercises and advice to become fit for the future following child birth, please see the Pelvic Obstetric and Gynaecological Physiotherapy’s booklet below.
Pelvic Floor Exercises
Hormonal and weight changes during pregnancy can place extra stress on the pelvic floor muscles. Make sure you exercise these muscles regularly to prevent any leakages.
Check out the video and/or the Pelvic Obstetric and Gynaecological Physiotherapy’s booklet below for further advice.
- https://www.youtube.com/watch?v=v731EXFR2k4
This video was produced by NHS Highland in conjunction with Association for Continence Advice - The Pelvic Floor Muscles – a Guide for Women booklet
If you are struggling with your exercises or any pelvic health issues seek help from your local GP, physiotherapist or nurse.
Web Links
This Mum Moves website – https://thismummoves.co.uk/
Partner Resources
Everyone has feelings of anxiety at some point in their life. Often, dads and partners are often overlooked when it comes to postnatal health and mental health. In some cases, you may feel worried and anxious about being a parent and if you will be good enough. This is similar to what mothers experience.
During times like these, feeling anxious can be perfectly normal. However, some people find it hard to control their worries. Their feelings of anxiety are more constant and this can often affect their daily life.
See links to the websites below which may help you to understand what you are feeling and offer some support.
Dads Matter – Provide support for dads
Local Leaflets for Glasgow North and North Lanarkshire
Baby Buddy – Aims to empower parents and care-givers to build their knowledge and confidence for the crucial first five years of their child’s life, when foundations are laid.
Mind – Information and support for mental health
Safer Sleep Guide
Patient Information Leaflets
- Postnatal Recovery Advice After Caesarean Section
- Postnatal Recovery Advice After Vaginal Delivery
- Induction of labour – coming soon
- PV bleeding – coming soon
- Vaginal Birth After Caesarean (VBAC)
- EROSS – coming soon
Postnatal
Infant Feeding
For guidance and advice on infant feeding, visit out infant feeding page. For healthy weaning recipes and feeding advice, visit our infant nutrition page.
BadgerNotes
What is BadgerNotes?
BadgerNotes is an online portal and app that allows you to access your maternity records over the internet through your PC, tablet device or mobile phone.
The information that you view is generated in real-time from your hospital-based maternity system, using details entered by your midwife or other health professionals involved in your care. The App is used to signpost you to relevant information regarding your pregnancy .
What are the benefits?
BadgerNotes have replace handheld records.There are a number of benefits to using BadgerNotes, over paper notes, such as:
- Information can be shared with you directly from the maternity system
- Records can be easily updated at each maternity visit or appointment
- Midwives do not have to double enter data onto paper handheld notes
- Only those with the correct login details are able to access the notes.
You can add information regarding:
- Yourself, such as your occupation and family history. This can be discussed with your midwife at your booking appointment
- Your plans and preferences for birth
- Feedback regarding your antenatal care, labour and birth experiences.
How secure is it?
- All information is held securely and cannot be accessed without the correct login details (similar to internet banking).
- BadgerNotes is powered by BadgerNet, the same secure platform used by healthcare professionals involved in your maternity care.
How to access BadgerNotes
Your midwife will provide you with a security phrase and record your contact details, including your mobile phone number and email address
Using a mobile phone
iPhone
- To access the service on your iPhone, please search for the BadgerNotes app in ITunes and download
- Once downloaded, tap on the icon in your home screen to open.
Android
- To access the service on your smart phone, please search for the BadgerNet Maternity Notes app in the Google Play store and download
- Once downloaded, tap on the icon in your home screen to open.
Using a PC or tablet
- You can login to the BadgerNotes website by navigating by clicking this link: net
- After entering your email address and security phrase, the system will ask for a confirmation code. This will be text to you
- If using a tablet device, after entering your confirmation code you will need to set a PIN code
- You are ready to view your records.
For more information, please see: A whistle-stop tour of the Badger Notes app. This video shows you how to create an account, and the key features of the Badger Notes app.
Patient Video Guide to BadgerNotes
View the video on YouTube: https://www.youtube.com/watch?v=cM1xDmEnWys
Maternity and Neonatal Psychological Interventions Service (MNPI)
The Maternity and Neonatal Psychological Interventions Service was established in 2021. It is our mission to provide a service that supports well-being of women, their infants, partners and families in Maternity and Neonatal Settings in Lanarkshire.
The service provides expertise from Clinical Psychologists, an Advanced Specialist Midwife and a Mental Health Practitioner. We use evidence-based approaches to understand and help when people experience difficult thoughts or feelings that are affecting their wellbeing and making it harder to do the things that they need or want to do.
- Service phone number – 01698 366346 (direct dial) or 01698 361100 (Main switchboard) extension 6346
- MNPI website
What are Maternity and Neonatal Psychological Interventions Teams? How can they help me?
For more information visit:
CONTACT
University Hospital Wishaw
50 Netherton Street
Wishaw
ML2 0DP
Tel: 01698 361100
Visiting Hours
Maternity:
- 3pm – 5pm & 6pm – 8pm.
- Birthing partners welcome 9am – 9pm
Neonatal unit:
- 3pm – 4pm & 730pm – 830pm.
- Parents welcome anytime. Strictly 2 visitors to each cot at any one time
Service Staff & Contact Numbers
- Maternity scan department – 01698 366340
- Early pregnancy assessment unit (EPAS) – 01698 366217
- Wishaw maternity day bed unit – 01698 366246
- Airdrie maternity day unit – 01236 763298
- Hairmyres Day bed unit – 01355 584502
- Maternity triage – 01698 366210
- Postnatal ward – 01698 366220/ 366221
- Antenatal ward – 01698 366231
- Alongside midwifery unit – 01698 366230
- Labour ward – 01698 366240/ 366241
- Transitional care unit – 01698 366243
Your Feedback - comments, concerns and complaints
NHS Lanarkshire is committed to improving the service it provides to patients and their families. We therefore want to hear from you about your experience. If you would like to tell us about this please visit our feedback page.
TRAVEL DIRECTIONS
How to Find Us
The maternity unit is situated on the second floor of the hospital (level2). During the day you can access the maternity unit by entering the hospital through the main entrance.
Between the hours of 21:45 and 06:00, when the main entrance is closed, you may use the Maternity entrance situated at the end of the hospital at Glasgow Road. An intercom system is in operation here.
By car
The hospital is just off the A721 Glasgow Road on Netherton Street, Wishaw.
The main entrance is on Netherton Street and the visitor car park is in front of the main entrance.
Disabled parking facilities are available.
By public transport
Visit the First Group website to plan your bus journey.
For times of train services to Wishaw, visit the Scotrail website.
Public transport information is available from the Traveline Scotland website or telephone: 0871 200 22 33.
Taxi Free Phone
There is a taxi phone line at the main entrance of the hospital.
Ambulance Transport
If you think you may be eligible for ambulance transport please contact the Patient Ambulance Booking Service which is provided by the Scottish Ambulance Service.
Contact the service within four weeks, but no later than 48 hours, prior to your appointment date on 0300 123 1236.
Lines are open 9am – 4.30pm, Monday to Friday.
An advisor will ask you a series of questions to determine your ambulance transport requirements, please have your letter or card handy when you call.
For more information please read the Are you eligible for ambulance transport? leaflet. This leaflet is also available in other formats on the Scottish Ambulance Service website.

