Dietary advice following an Oesophagectomy or Gastrectomy
Information for patients
NHS Lanarkshire Nutrition and Dietetic Department
PIL.OESOPH.19_00744.L
Your dietitian
Good nutrition is an important part of your treatment and often patients can find it challenging getting the diet right.
Your dietitians are there to support you before surgery, throughout your hospital stay and afterwards once you are discharged, as required.
This diet sheet is to be used as a guide only. If you have any specific concerns relating to your diet or you are experiencing unintentional weight loss please speak to your dietitian or contact your GP or surgical team.
Type of surgery
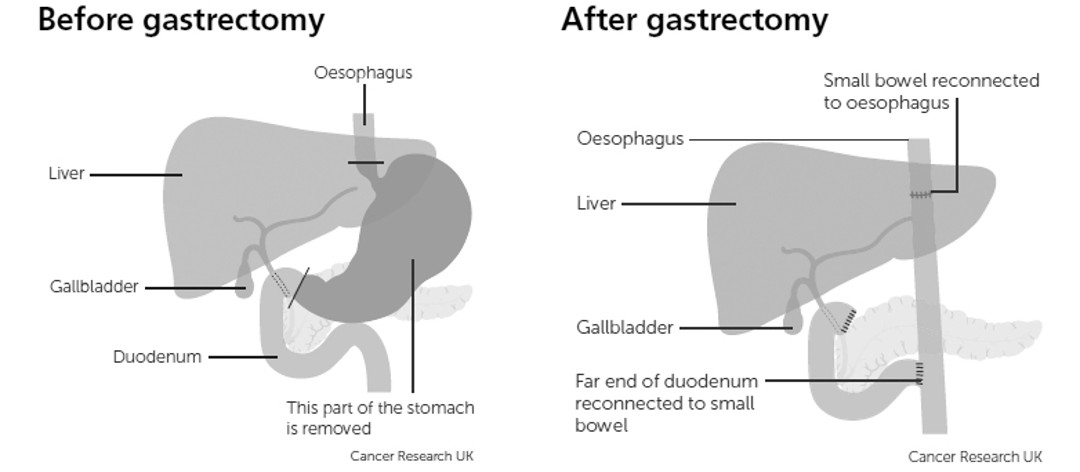
Subtotal gastrectomy
The removal of part of the stomach
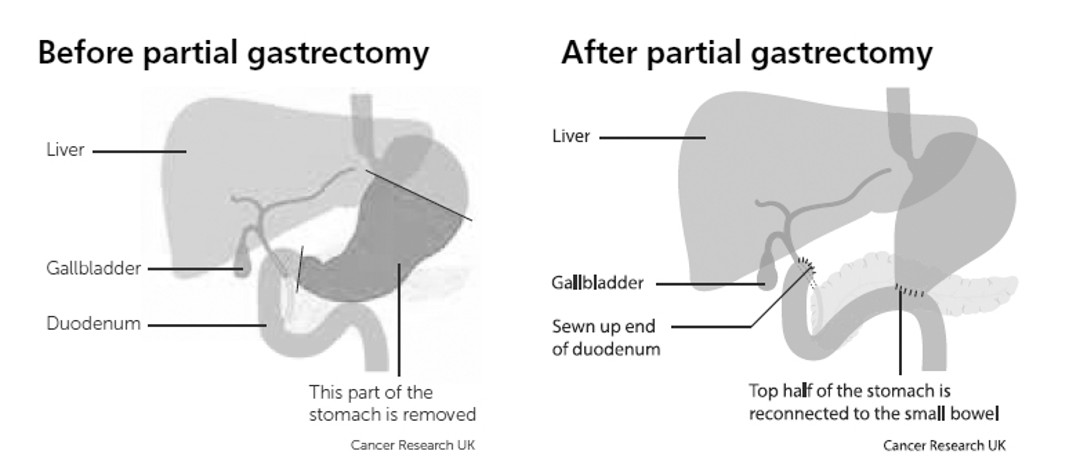
Total gastrectomy
The removal of the whole stomach
Type of surgery
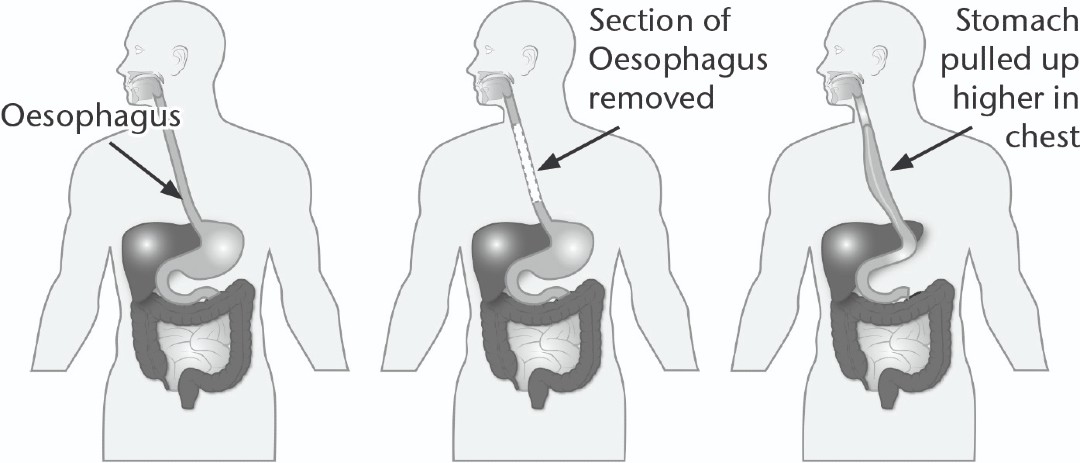
Oesophagectomy
An oesophagectomy involves removal of part/or all of the oesophagus. It may also involve removal of the top part of the stomach.
During an oesophagectomy a feeding tube may be placed into your small bowel (jejunostomy) to provide nutrition following surgery. This can be used as a sole source of nutrition and then
to supplement your nutritional intakes as you recover.
Your dietitian will work alongside you to reduce the amount of feed given via this tube as your oral intakes improve. This feeding tube will normally remain in place for at least 6 weeks after surgery or until it is no longer required. If you are not having feed at home you should continue to flush the tube twice daily with cooled boiled water until the tube can be removed. Training will be provided on all aspects of tube care by our specialist Abbott Nurses.
After your surgery
Your surgical team will advise you when you can resume eating and drinking. However below is a guide of how and when food and drink would normally be introduced
- Step 1 (normally 5-7 days after surgery)
- Sips of water and clear fluids (which includes diluting juice, juice based supplement drinks, black tea and coffee)
- Step 2 (normally 6-8 days after surgery)
- Free fluids (which can include) all of the above and milk, milk based supplement drinks, ice cream, yoghurt or thin soup with no lumps.
- Step 3 (normally 7-10 days after surgery)
- Soft sloppy diet for the next 4-6 weeks following your operation
Importance of nutrition following surgery
It is important to maintain good nutritional intakes at all stages of your treatment especially after surgery. This will help with your recovery, aid wound healing and will also help minimise weight loss.
After your operation you won’t have the same reservoir for food. For this reason it is important to eat little and often to ensure your body gets the nutrition it needs, in portion sizes you are able to tolerate.
Guide to following a soft sloppy diet
When introducing solid foods start off with cereals such as weetabix or porridge with lots of milk, very soft moist foods such as mashed potato in gravy, scrambled eggs or blended soups/pureed meals and semi-solid puddings such as custard, rice pudding, jelly, ice-cream and yoghurt. You can then increase the variety of soft/moist foods as tolerated (see pages 7 – 8 for meal ideas).
Key dietary advice when introducing soft sloppy diet:
- Start with palm sized portions
- Foods should be easily mashed with a fork and moist
- Chew your food well and avoid swallowing large, hard lumps
- Add sauces, gravy and butter to moisten foods
- Foods should not contain sharp edges, skins, pips or seeds.
Follow a little and often meal pattern
- Eat 5-6 small meals per day, eating every 2 hours
- Try using a side plate for main meals to ensure small portion sizes and not becoming too full
- Sit upright when you eat and for about 30 minutes after a meal
- Drink 8-10 cups of fluid per day, which can include nourishing drinks, throughout the day. Try to only have small sips of fluid with meals and have the rest in between meals
- If you suffer from reflux avoid eating late and night and ensure you are propped up when sleeping.
Meal ideas
Breakfast
- Cereal or porridge with full fat milk and ground almonds
- Full fat yoghurt with mashed banana
- Omelette, poached or scrambled eggs (2 eggs)

Main meals
- Poached fish with mashed potato
- Savoury mince (beef, lamb, poultry, soya) with mashed potato and gravy
- Cottage/shepherds pie
- Macaroni Cheese with plenty of sauce
- Pasta/spaghetti bolognaise, lasagne
- Corned beef hash
- Stews, casseroles, curries made with tender meat and well cooked vegetables
- Omelette, poached or scrambled eggs
- Skinless sausages with mashed potato and gravy
- Dahl
- Jacket potato (without skin) and tuna mayonnaise and/or cheese

Puddings
(can be eaten 30-60 minutes after eating if you are feeling too full)
- Milky puddings i.e. Rice pudding, semolina, sago, tapioca, custard
- Stewed fruit, soft tinned fruit or mashed banana with custard, double cream or ice-cream
- Full fat yoghurt, mousse, trifle, tiramisu, crème caramel or instant whip
- Jelly and ice-cream

Snacks
- Cereal or porridge with full fat milk and ground almonds
- Glass of fortified milk
- 2 biscuits (dipped in tea/coffee to soften) or piece of cake
- Full fat yoghurt with mashed banana
- Mashed avocado, Houmous, smooth butter, soft cream cheese on soft crackers (e.g. Ritz ©)
- Prawn cocktail
- Lentil/cream of chicken/cream of tomato soup
- Oral nutrition Supplement

Nutritional supplements and nourishing drinks
Oral nutrition supplements
Oral nutrition supplements are high energy/high protein drinks that can be provided by the dietitian to supplement your oral intakes as required. These are usually juice based or milkshake style drinks.
Fortified milk
This can be used instead of ordinary milk for added nourishment.
If you do not like full-fat milk, fortify semi-skimmed milk instead.
4 tablespoons of dried milk powder
600ml/1pint full fat milk
- Add the powder to a small amount of milk at first to make paste and then add the rest of the 600ml
- Keep this in the fridge and use in milky drinks, sauces, puddings and cereals
For more information on nourishing drinks ideas please ask your dietitian for our nourishing drinks diet sheet
Dumping syndrome
Dumping syndrome is a term used to describe a group of symptoms that you may experience after surgery. This happens when food moves too quickly into the small intestine and symptoms can present immediately after eating or up to 4 hours following a meal.
Early Dumping Syndrome
(Can occur 10-30 minutes after eating)
Symptoms include: nausea, bloating, abdominal cramps, diarrhoea, dizziness, feeling lethargic and rapid heart rate.
Late dumping Syndrome
( Can occur 1-4 hours after eating)
Symptoms include; sweating, shakiness, having a hard time focusing and hunger. Symptoms of late dumping syndrome are from an imbalance in your blood sugar levels.
Tips to avoid dumping syndrome
- Eat small, regular starch based meals
- Avoid large volumes of fluids with meals
- Limit simple, added sugars i.e. Sugary/fizzy drinks, cakes/biscuits and sweets. Use sweeteners where necessary.
- Take your time with eating and chew foods well
If you experience these symptoms you may feel better if you lie down for 30minutes and eat a snack.
| Foods to avoid | Foods to choose |
|
Sugar |
Artificial sweetners |
| Sugary drinks | Diet Low calorie drinks |
| Jam marmalade honey | Low sugar jam marmalade Smooth peanut butter |
| Sweets cakes and biscuits | Plain biscuits |
| Tinned fruit in syrup | Tinned fruit in juice/water |
Vitamin and mineral deficiencies
Surgery to your oesophagus and/or stomach can increase the risk of vitamin and mineral deficiency due to dietary restrictions, malabsorption or the surgery itself.
You may become deficient in calcium, iron or vitamin B12, due to decreased absorption, which can lead to weakening of the bones and anaemia. Your doctor should be monitoring your blood levels annually (as a minimum) and recommending supplementation as required.
Life after surgery
Once you have recovered from your operation and your weight is stable you should be able to return to a normal healthy diet as able. Many patients will need to maintain a little and often approach to food and fluids due to having a reduced storage capacity.
It is not uncommon for people to find life after surgery emotionally challenging as they process the changes they have been through. If this is something you are struggling with your GP or specialist nurses will be able to discuss this with you and advise you on any support groups in your area.
Further Information
You should be referred to see the diabetes dietitian for further information and individual advice.
Pub. date: March 2023
Review date: March 2025
Issue No: 03
Reference: PIL.OESOPH.19_00744.L
23_10256
If you need this information in another language or format, please e-mail:





