Gastroparesis and Diet
Information for patients
NHS Lanarkshire Dietetic Department
PIL.GASTRO.19_19725.L
Gastroparesis
Gastroparesis, or delayed gastric emptying is a condition affecting how the stomach works. If you have gastroparesis, your body takes longer to pass food out of the stomach down into the intestine.
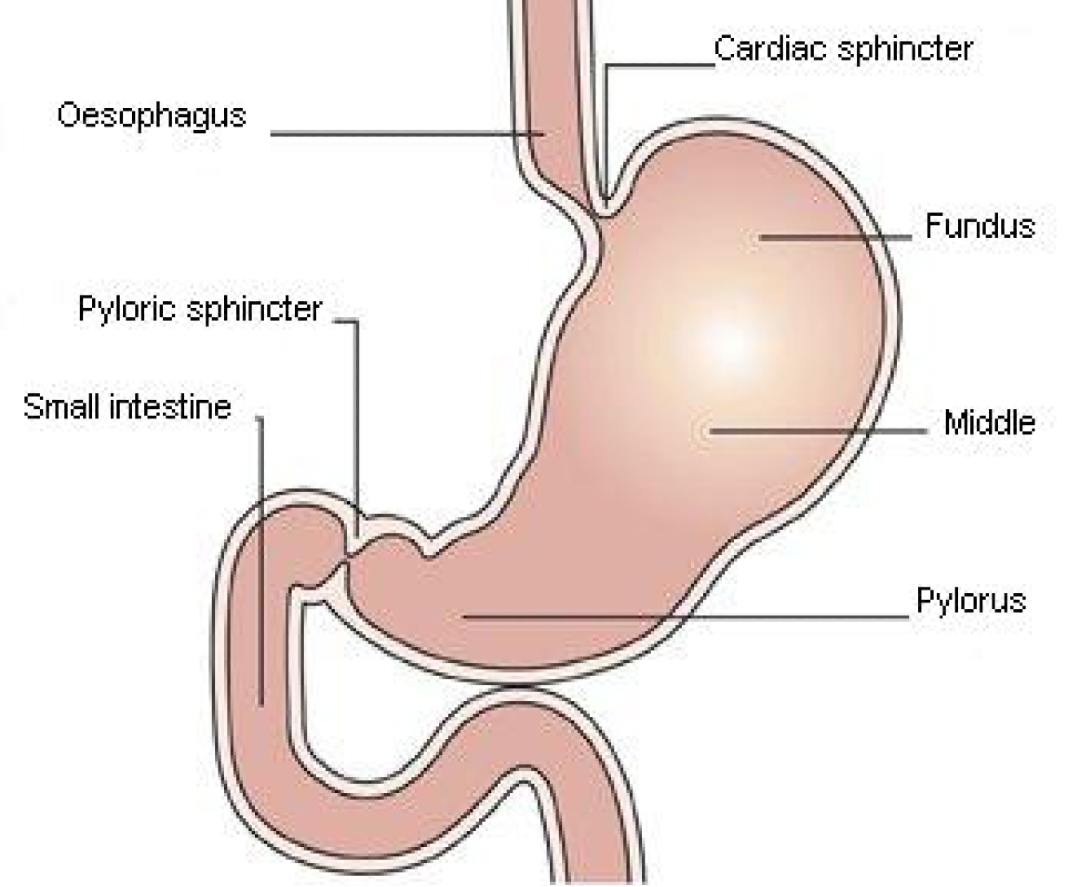
The stomach mixes food into a liquid. This mixture then moves through a valve called the pyloric sphincter into the intestine where digestion continues.
Symptoms
You may have some or all of the following symptoms:
- nausea (feeling sick)
- vomiting
- feeling full quickly when eating
- loss of appetite
- weight loss
- bloating
- abdominal pain or discomfort
- heartburn
Causes
Gastroparesis happens because the muscles and nerves that are meant to make the stomach empty don’t work properly.
There are different reasons why this can happen:
- High blood sugar levels (hyperglycaemia) caused by poorly controlled diabetes can damage nerves, including those affecting stomach emptying
- Some types of surgery such as weight loss (bariatric) surgery or partial gastrectomy (where part of the stomach is removed)
- Medications such as opiate painkillers like morphine and antidepressants
- Other health conditions such as Parkinson’s, scleroderma and amyloidosis
- Sometimes we don’t know what the cause is – this is known as idiopathic gastroparesis
Diagnosis
You may be asked to have some investigations to rule out other medical conditions with some similar symptoms to Gastroparesis. These investigations might include a pH study, endoscope, CT scan, ultra sound scan or colonoscopy. Different people may require different tests. You can find out more about these tests from your doctor.
If your doctor thinks you may have Gastroparesis, you may be asked to have a gastric emptying study. This involves eating a small amount of radioactive food that is detected on a scan. The scan shows how fast the radioactive food moves from the stomach into the small intestine.
Treatment
Lifestyle and well-being
- Stress and anxiety may worsen your symptoms
- Take time to relax, for example using relaxation tapes, yoga, aromatherapy or massage
- Take regular exercise such as walking, cycling or swimming
- If you would like help with this, please speak to your GP
Medication
Medications such as opiate painkillers (e.g. morphine) and antidepressants can make your symptoms worse. Ask your doctor whether alternative medications are available.
Glycaemic control
If you have diabetes, keeping your blood sugars within your target range is very important. High blood sugars can slow the rate of stomach emptying which may make symptoms of Gastroparesis worse. If you would like support with this, please contact your GP, Diabetes Nurse or a Dietitian.
Diet
Dietary modifications are an important part of treatment.
- Think about when and how you eat:
- Eat small regular meals – aim for six mini meals daily
- Avoid rushing and chew food well
- Eat sitting down in an upright position
- If possible, avoid lying down for an hour after meals
The types of foods you eat may also help reduce your symptoms:
Texture modification
Softer or pureed foods may be easier to manage. Ask to be referred to a Dietitian if you would like advice about how to make these types of meals nutritious and varied.
Fat
Fat is an essential part of our diet and it provides our bodies with important energy and vitamins; however, high fat foods may make your symptoms worse. If this is the case, try to avoid large portions of these foods. Different people can tolerate different amounts.
High fat foods include: chips, fast foods, pies, batter, cheese, pizza, creamy sauces, snacks such as crisps, chocolate, cake and biscuits, spreads and cooking oils, and fatty meats such as burgers and sausages.
For more information visit the BDA website.
Malnutrition
If you have a small appetite or have unintentionally lost weight, you may be at risk of malnutrition. If this is the case, you may be advised to eat more foods that are high in fat and sugar. This is an important way of increasing your nutritional intake. Research has found that liquid forms of higher fat foods such as milkshake are easier to manage. If you are diabetic, speak to a Dietitian before increasing your sugar intake as this can cause hyperglycaemia (high blood sugar levels).
For more information visit the BDA website.
Fibre
- Fibre is important for normal gut function and many foods containing fibre are a good source of vitamins and other healthy nutrients. If you have Gastroparesis, it is important to eat the right amount of fibre. Too much or too little may make your symptoms worse. How much you need varies from person to person.
- Foods high in fibre include: fruits, vegetables and foods made from wholegrains such as wholemeal bread, brown rice and pasta, and some crackers and breakfast cereals
- Make any changes to your fibre intake slowly until you feel a benefit. Stop and seek advice if your symptoms worsen
| Too much fibre | Too much fibre may slow the rate of stomach emptying. In gastroparesis, this could mean food takes even longer to leave the stomach. | Cooking food thoroughly, chewing well or blending fibrous foods may help. You may benefit from reducing your fibre intake. |
| Not enough fibre | Not eating enough fibre can increase your risk of constipation, which can make gastroparesis worse. | Increasing your fibre and fluid intake may improve your symptoms. |
Drinks
- Limit alcohol to no more than two units per day. Have at least two alcohol free days a week
- Reduce caffeine-containing drinks such as tea, coffee, cola and Iron-Bru, aim for no more than two mugs (three cups) a day
- Avoid fizzy drinks
- Drink at least eight cups of fluid per day, especially water or other noncaffeinated drinks, for example herbal teas
Pub. date: October 2021
Review date: October 2023
Issue No: 01a
Reference: PIL.GASTRO.19_19725.L
21_27928
If you need this information in another language or format, please e-mail:




