Guidelines for Best Practice for Clean Intermittent Catheterisation in Children and Young People
Information for patients
NHS Lanarkshire Neonatal Department
PIL.GUIDES.21_23212.W
Objectives
The aim of this document is to offer guidance on best practice to all carers and professionals especially those in the community who provide Clean Intermittent Catheterisation (CIC). It provides guidance from the Best Practice Statement – Urinary Catheterisation and Catheter Care (NHS Quality Improvement Scotland, June 2004) and incorporates advice from current local practice.
Rationale
CIC is a normal part of daily living activity for some young people with bladder problems. This procedure has a considerable positive impact on the young person’s wellbeing and personal dignity and maintains a healthy urinary tract.
Introduction
This document has been developed using evidence based practice and references are sited at the end. This is for the use of the individual young person, parents, carers, nurses and support staff, to ensure appropriate use and teaching of Clean Intermittent Catheterisation (CIC). Many people need the support of continence products – like catheters – to help them manage their continence and maintain a healthy bladder. CIC allows many individuals to gain control of their bladder and give them the opportunity to become self caring. CIC may be a short or long term intervention. The procedure involves the introduction of a catheter into the bladder to remove urine, once the bladder is empty the catheter is removed. CIC is performed as often as required to prevent prolonged retention of urine and to assist continence. CIC can be performed using natural or artificially created channels. CIC has a lower infection rate than an indwelling catheter and should always be used if it is clinically appropriate and a practical option for the individual. CIC requires to be carried out at regular intervals as recommended by health care professional. Health and education support workers may therefore be required to provide assistance or carry out this procedure while the young person is at school. It has been demonstrated that the skills required to complete this task are well within the scope of all carers for the young person including parents, health care and education support workers working in the home or the community.
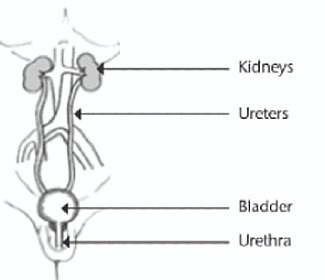
Components of the Urinary System
Indications for clean intermittent Catheterisation (list is not inclusive)
- To ensure the bladder is emptied completely
- To irrigate the bladder
- To administer medication within the bladder.
Impaired Bladder Function – Causes
There are two types of bladder emptying problems for which CIC is indicated:
- Inability to empty bladder due to poor bladder action
- Inability to empty bladder due to obstruction
A mixture of these two can occur in the same young person. Below are some of the conditions for which CIC is recommended – this list is not inclusive.
- Congenital malformations.
- Bladder outflow obstruction – this happens when base of bladder is partially or completely blocked and reduces or prevents flow of urine into the urethra due to anatomy or stricture.
Associated Bladder Problems
- Bladder Over Activity – the bladder muscle contracts spontaneously leading to leakage of urine and in some cases backflow into the kidneys.
- Incomplete Bladder Emptying – if the bladder cannot be emptied fully, the urine that is left in the bladder is known as residual urine. Bacteria can grow quickly in this residual urine, causing a urinary tract infection.
- Urinary Tract Infections – it can be completely normal for anyone to have some bacteria in their urine. Those who perform CIC may have an even higher bacteria count in their urine. If the young person experiences symptoms such as temperature, vomiting and pain, this may be a urinary tract infection and a course of antibiotics will be prescribed. Serious recurrent and untreated urinary tract infections may cause damage to the kidneys.
- Urinary Reflux – backflow of urine from the bladder to the kidneys. Young people with reflux problems are at greater risk of urinary tract infections and kidney damage.
- Impaired Kidney Function – repeated upper urinary tract infections and prolonged urinary reflux may damage the kidneys over time. There is a risk that this may reduce the function of the kidneys long term.
Methods of Clean Intermittent Catheterisation
- Urethral – urethral catheterisation is a routine procedure performed with a sterile catheter inserted via the urethra into the bladder for the purpose of urine drainage, administering medications or irrigation of the urinary tract.
- Mitrofanoff – this is a surgical procedure to produce a stoma, an artificial channel into the bladder through the skin. A sterile catheter can be inserted through this to empty the bladder. The stoma which can look like an extra tummy button but not always. In some cases, this is combined with an operation to enlarge the young person’s bladder (bladder augmentation).
Types of Catheters (Catheters come in many types, materials and sizes)
- Flexible silicon or plastic tube.
- Lubricated with gel or require the lubrication to be activated by water.
- Normal drainage is usually achieved by using a catheter size between CH06 TO CH12.
- Correct size is the smallest possible for providing adequate drainage.
- Larger catheters can cause more leakage and damage and should only be used in special circumstances such as with an indwelling catheter insitu.
Infection Control – General
- A clean environment should be maintained at all times.
- Catheter equipment should be stored
- in a dry, cool, dark place, out of direct sunlight.
- unopened in manufacturer’s protective boxes/wrapping to prevent damage and ensure the integrity/sterility of the product.
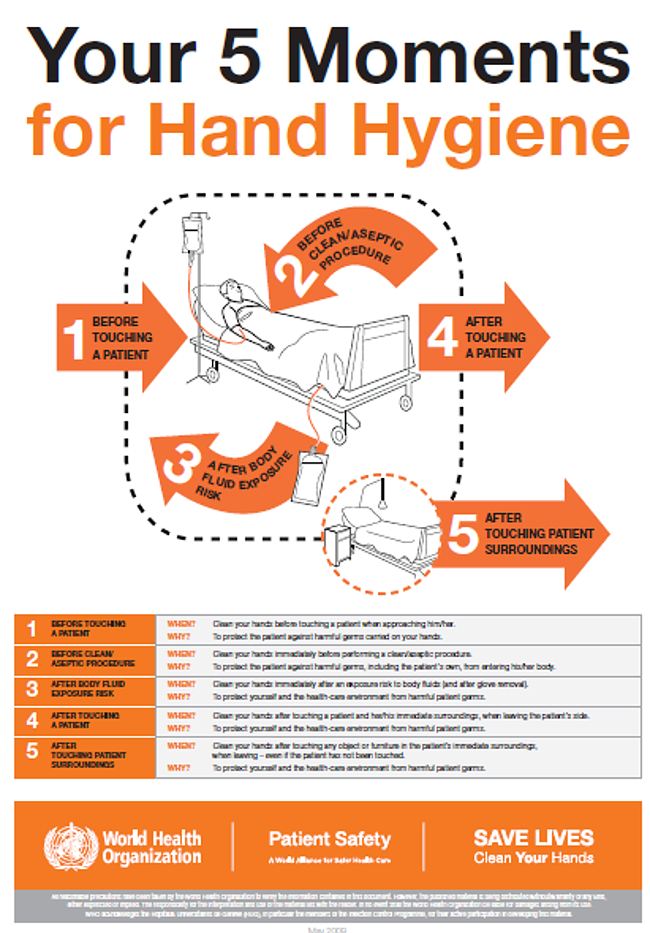
- Hand hygiene is appropriate for care, as hand transfer is a major factor in the current risk of infection to patients.
- Effective hand drying is carried out before catheter procedures, as friction created while drying further assists the removal of bacteria. Failure to dry hands can lead to cracked skin and breeding grounds for bacteria.
- Personal protective equipment (PPE) such as aprons and gloves should be used for all activities that have been assessed as carrying a risk of exposure to blood and body fluids/
- Single use gloves should be kept in manufacturer’s box and only removed as required.
- All equipment used for these procedures should be single use wherever possible.
- All waste should be disposed of according to local policies and guidelines.
Infection Control – Hand Hygiene
- Follow principles of good hand hygiene before, during and after procedure.
- Cover all cuts and abrasions with water-proof dressings.
- Keep nails short and clean; do not wear nail varnish, artificial nails or extensions.
- Wrist-watches, stoned jewellery, bracelets or rings (other than 1 plain band) in the clinical environment. Hand jewellery will impede the performance of effective hand hygiene thus increasing the risk of infection.
- Sleeves should be worn above the elbow.
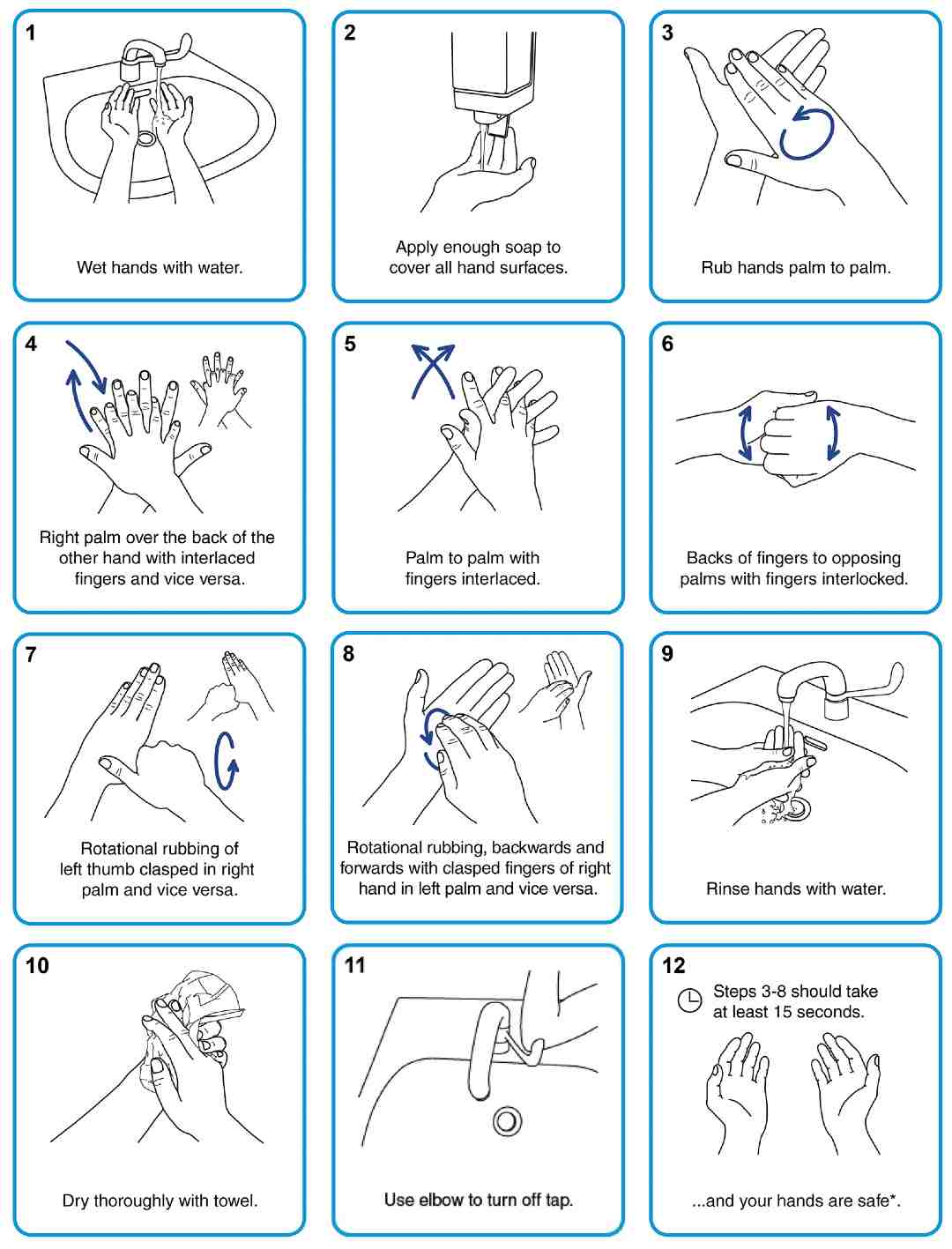
How to Wash Hands
Procedural Guideline – General
Before, during and after procedure ensure the young person’s dignity is maintained at all times, considering legal, moral, cultural and religious beliefs.
- Select dedicated location which is appropriate for performing the procedure.
- Young person has consented and is comfortable and happy for procedure to take place.
- Appropriate equipment including apron, gloves, goggles, catheter and drainage container is available.
- Ensure procedure is fully explained using appropriate language.
- Ensure the young person is in a suitable position for the procedure to be performed.
- Remove and loosen clothing where appropriate.
- Wash hands thoroughly.
- Prepare catheter, check expiry date and lubricate if necessary.
- Put on protective personal equipment eg: gloves, apron as required.
- Ensure genital area is cleaned using unfragranced soap or wipes, in downwards strokes, before insertion of catheter.
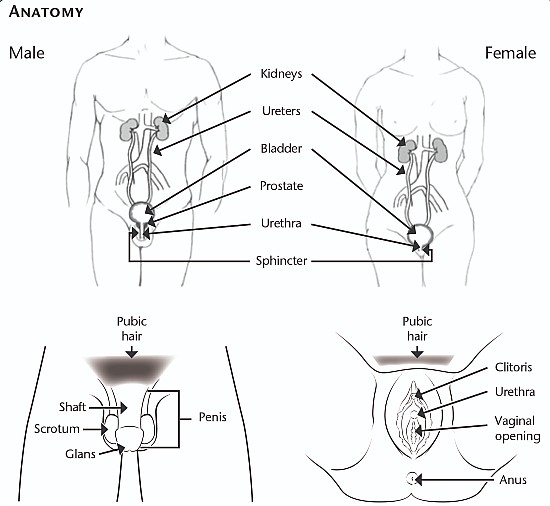
Procedure – Male Urethral Catheterisation
- Hold penis on sides, perpendicular (at 90-degree angle) to the body, straightening the urethra.
- Retract the foreskin gently where appropriate.
- Slide lubricated catheter into the opening of urethra, at tip of penis.
- Gently insert the catheter and advance it slowly towards the bladder.
- There may be resistance, do not pull catheter in and out, encourage young person to relax and breathe deeply until muscle relaxes.
- Advance catheter and massage bladder until urine starts to flow into the toilet, container or nappy.
- Advance catheter for further 1-2 cms. Hold in position until urine stops flowing.
- Remove catheter gently in small steps to ensure bladder is empty.
- If, as the catheter is being removed, urine starts to flow again, stop withdrawal until urine flow stops.
- Replace foreskin over glans of penis. Wash and dry penis, replace clothing as appropriate.
- Record time of catheterisation and amount of urine obtained if appropriate.
- Discard all waste following local policies and guidelines for clinical waste.
Procedure – Female Urethral Catheterisation
- Using fingers separate the labia and pull gently upwards to visualise the urethral meatus.
- Locate the urethra, which is below the clitoris and above the vagina.
- Slide lubricated catheter gently into the opening of urethra.
- Advance it slowly towards the bladder, guiding it upwards as if towards tummy button.
- There may be some resistance as the catheter tip reaches the bladder neck, continue to advance the catheter gently but firmly until the sphincter relaxes.
- Advance catheter until urine starts to flow into drainage container.
- Continue to advance catheter for further 1-2 cms.
- Hold in position until urine stops flowing and bladder is empty.
- If, as the catheter is being removed, urine starts to flow again, stop withdrawal until urine flow stops.
- Wash and dry genital area, replace clothing as appropriate.
- Record time of catheterisation and amount of urine obtained if appropriate.
- Discard all waste following local policies and guidelines for clinical waste.
Procedure – Mitrofanoff Catheterisation
- Remove ACE stopper if present.
- Insert the catheter gently into the mitrofanoff until you meet resistance and then give it a firm push to guide it further into the bladder.
- Allow urine to drain freely.
- When urine stops flowing, remove catheter.
- Dry stoma site if required and insert ACE Stopper (if used) and replace clothing.
- Record time of catheterisation and amount of urine obtained if appropriate.
- Discard all waste following local policies and guidelines for clinical waste.
Problem solving – Female Urethral Catheterisation
| Problem | Solution |
| Genital area red or inflamed, or discharge present |
|
| Unable to pass catheter due to resistance |
|
| Unable to obtain urine on insertion of catheter into urethra |
|
| Bleeding evident on catheter insertion |
|
| Unable to pass catheter due to spasm |
|
| Unable to withdraw catheter |
|
| Stoma site red, inflamed or bleeding |
|
| Site leaking and sore |
|
| Unable to insert catheterUrine leaking from stoma between catheterisations |
|
| Bleeding evident on catheter insertion |
|
Problem Solving – Urine
| Problem | Solution |
| Pale, straw coloured urine. No foul smell. No pain or discomfort. |
|
| Concentrated. Dark urine, strong smelling. No pain or discomfort |
|
| Blood visible in urine. Foul smell. Pain and discomfort |
|
| Bleeding evident on catheter insertion |
|
Holidays and Travelling Abroad
Essentials for Holiday
- Order supplies for length of holiday and include extra to allow for delays.
- Arrange standby course of antibiotics from GP.
- Obtain travel letter from GP or Specialist Nurse.
- Ensure appropriate travel insurance is in place.
Essentials for Travelling Abroad
- If booking flights, ensure adequate baggage allowance for supplies.
- Consider the hygiene needs of the country you are visiting.
- Appreciate the need to carry medication and catheters in hand luggage.
Contact Information
If you have any questions in relation to this training pack, please do not hesitate to contact the Integrated. Community Children’s Nursing Team in NHS Lanarkshire.
Team Leader
Integrated Community
Children’s Nursing Team
NHS Lanarkshire
ccnteam@lanarkshire.scot.nhs.uk
Practice Development Centre
www.lanpdc.scot.nhs.uk
Wishaw General Hospital
Netherton Street
Wishaw, ML2 0DP
Community Children’s Nurse: 01698 366035

Review date: December 2023
Issue No: 01
Reference: PIL.GUIDES.21_23212.W
If you need this information in another language or format, please e-mail:





