Asthma
Information for patients
NHS Lanarkshire Neonatal Department
PIL.ASTHMA.06391.L
Introduction
This information has been written for parents who have children with asthma. It tells you a bit about asthma and its treatment. We hope you will like it and find it helpful. If we have missed out something special that you want to know, ask the doctors or nurses looking after your child. Please write down any questions you have for the doctors or nurses. Take them with you the next time you visit the doctor or nurse.
Finding out more about Asthma
You can get more help and advice by calling:
Your General Practitioner or Practice Nurse OR Paediatric Unit at University Hospital Wishaw
Respiratory Nurse Specialist
- Call 01698 366679 Monday to Friday 9am-5pm
A new website for parents of children with asthma
You may want to know about benefits you can claim for your child. There is a leaflet called “Asthma – what benefits can I claim”. You can get a copy from Asthma UK website.
Part 1 – What is Asthma
Asthma is a disease which affects the airways and breathing. It can affect people of all ages, but is most common in childhood. In Britain, between 10-20% of children have asthma.
What happens in Asthma?
The lining of the airways becomes swollen and inflamed. The airways produce thick mucus. The muscles around the airways tighten and make the airways narrower. This blocks the flow of air into the lungs and makes it difficult to breathe. People with asthma sometimes say it is “like breathing through a straw”.
How does the doctor know your child has Asthma?
There is no definite test for asthma. There are no blood tests or X-rays that can show that your child has asthma. The doctor will listen to your story of their symptoms and when they happen and examine your child carefully. From this the doctor can recognise the patterns seen in asthma.
What are the most common Asthma symptoms?
- cough
- difficulty breathing
- chestiness
- noisy breathing
- wheezing
- chest tightness or pain
When are Asthma symptoms most likely to happen?
In children, asthma symptoms are most likely to happen with colds, at night or during exercise.
Asthma triggers
People with asthma have airways that can be sensitive to lots of different things. These different things are called “triggers”. When someone with asthma comes into contact with their trigger, their asthma is started off. The airways tighten up, become swollen and produce too much mucus.
Most children’s asthma is set off by catching a ‘common cold’, not by allergies.
Here are some triggers that people with asthma are sensitive to – which are your child’s triggers?
- colds/chest infections
- exercise/physical activity
- cigarette smoke
- cold weather
- changes in the weather
- laughing, crying or getting upset
- house dust (more later)
- animal fur/feathers
- pollens
- air pollution
Part 2 – Asthma medicines and devices
Good news
Children with asthma can lead a normal active life. This depends on avoiding triggers and finding the right doses of the right medicines for your child. Some famous people with asthma who lead very active lives include – Paul Scholes (footballer), Paula Radcliffe (marathon runner) and Laura Trott (Olympic Cyclist).
The two most common types of medicines for asthma are: preventers and relievers.
1. Preventers (usually Brown or Orange containers)
- Are all inhaled corticosteroids, or ‘steroids’ for short.
- Stop the inflammation and swelling in the airways which cause asthma symptoms.
- Give long lasting protection, and help prevent asthma attacks.
- The main ones are Clenil Modulite (beclomethasone) & Flixotide (fluticasone).
Importance of preventer
- Preventers do not work immediately. It can take a few weeks before you notice any improvement in your child’s asthma.
- Your child must take their preventer regularly every day without a break. Once the preventer starts to work, the airways become less inflamed and less sensitive to triggers.
- Do not stop using the preventer on good days because the airway can still be inflamed. Tell your doctor if you feel your child has not had any symptoms for some time.
2. Relievers (usually in blue containers)
- Relax the muscles around the airways.
- Work quickly within five to ten minutes.
- Give quick relief, not long lasting protection.
- Should be used when symptoms appear or before exercise.
- The most common are Ventolin (salbutamol) and Bricanyl (terbutaline).
- You do not get addicted to reliever medicines.
Tips for using your reliever
Use relievers early: Use early, at the first sign that your child’s asthma is getting worse. Watch out for your child’s early warning signs.
Take relievers before exercise: Most children with asthma get wheezy when running around. Children should use their reliever five or ten minutes before starting exercise.
Other Asthma medicines
Sometimes inhaled preventers are not enough to control asthma symptoms. Your doctor may then recommend other medicines to help. The most common are:
Combination Inhalers
- Seretide purple inhaler (Fluticasone & Salmeterol)
- Symbocort red inhaler (Budesonide & Formoterol)
- Tablets – Singulair (Montelukast) or Accolate (Zafirlukast)
- Steroid tablets – Prednisolone
Combination Inhalers contain a “protector”
- Protectors relax the muscles around the airways.
- They do this for a longer time than blue inhalers.
- They only need to be taken twice a day as part of the combination.
- They do not work immediately, so
- You should not use a protector or combination inhaler instead of your blue inhaler.
Singulair or Accolate
- These tablets are not steroids.
- They reduce inflammation in the airways.
- They need to be taken every day.
Steroid tablets
Your child may be prescribed a short course to cure an acute attack. Occasionally children with very severe asthma may need to take steroid tablets every day.
Prednisolone is the most common tablet.
A quick guide to Asthma Medicines
| Type | Common Names | What do they do? | How often should they be taken? | |
| Inhalers | Reliver blue | Salbutamol, Ventolin, Bricanyl | Relax the muscles around the airways | When needed |
| Preventer brown orange | Clenil, Modulite, Flixotide | Reduce inflammation & swelling in the airways | Every day | |
| Combination purple red | Seretide, Symbicort | Reduce swelling & relax the muscles around the airways | Every day | |
| Tablets | Non-steroid | Singulair, Accolate | Reduce inflammation & swelling in the airways | Every day |
| Steroid | Prednisolone | Reduce inflammation & swelling in the airways | During an acute attack or for very severe asthma |
Asthma devices and using them properly
Inhalers
Most asthma medicines are inhaled.
Using inhalers means:
- The medicine goes straight to the airways.
- Much smaller doses of medicines can be used.
- There are fewer side effects.
Asthma inhalers come in all shapes and sizes. They are often called devices.
To make sure young children get the medicine properly we use spacers. Commonly used spacers are:
- Aerochamber
- Paediatric Volumatic
Young children should always use a spacer with any inhaler as it is too difficult for them to breathe the medicine in properly, otherwise – they swallow it. With spacers the child can breathe in and out normally and still get the medicine.
Spacers are also used for emergency treatment with children of ALL ages. If you don’t have a spacer for your child ask your doctor for one.
- Accuhaler
- Easyhaler
- Turbohaler
Pictures of all of these asthma devices are below.
Spacers
- Volumatic Spacer for use with ventolin, flixotide, seretide, and clenil modulite

- Aerochamber suitable for any puffer

Dry Powder Devices
Accuhaler

Turbohaler

Easyhaler

Tips for remembering medication
- Almost everyone forgets to take medicine sometimes.
- The best thing to do is to give medicine as part of some other routine: e.g. brushing teeth, having a wash, getting dressed, with meals.
- You could also try keeping the preventer where you will always see it.
- If you feel that you forget the medicine a lot, tell your doctor or nurse.

What happens if my child does not take their preventer every day?
Preventers stop the inflammation and swelling in the airways which cause asthma symptoms. Forgetting or stopping the preventer medication for a few days means this protection will begin to disappear. Your child may then develop asthma symptoms again or have more frequent attacks. This may lead to your child needing more courses of steroid tablets.
My child has no asthma symptoms. Can I stop giving them their preventer?
When the preventer is working well your child may not have any asthma symptoms or need any reliever. However, the airway can still be inflamed so do not stop using the preventer on good days. If you feel your child has not had any symptoms for some time tell your doctor.
Tips for getting a young child/baby used to their inhaler
It is important to get your child used to their inhaler. Young children are not frightened of inhalers but can find them upsetting at first.
You might take at least a week getting your child comfortable with their inhaler and spacer before they take any medicine.
- For the first couple of days get your child used to the mask. Play some games with the mask – put it on top of child’s head, make it fall off. Let your child hold the mask and play with it.
- After a few days get your child used to the mask being placed over their nose and mouth.
- Next join the mask to the spacer. Hold this to your child’s face. Some parents sing a nursery rhyme while doing this. You can put stickers on the spacer to brighten it up.
- When your child is happy doing this, get them used to a short hissing noise when the mask is on their face. The medicine makes a noise when you press it and some children get a fright at this.
- Once your child is used to all of this, repeat twice a day.
Your child is now ready to be given the medicine.
Remember
- Always try to make it fun.
- If your child is not letting you use the inhaler, let them calm down and come back to it later on.
- If you are finding it very difficult to get your child to co-operate, speak with your Nurse for extra support.
- It is common for young children to fight their inhalers, this is normal behaviour but if it becomes problematic, your nurse can give you helpful tips to get the medicines into their lungs effectively!
- Don’t worry!
Giving your child’s medication
To give medicine to a baby:
- Get everything you need: inhaler, spacer device, mask.
- Shake the inhaler.
- Attach the inhaler to the spacer.
- Make sure your baby is in a comfortable position, lying on her/his back.
- Put the mask over your baby’s nose and mouth – press very gently to make a seal.
- Press the inhaler once and,
- Count ten breaths (watch for a breath hold and you may need to put a hand on their abdomen to help you count the breaths).
- Take the spacer away from your baby’s face.
- Take the inhaler out of the spacer. Leave 30 seconds between each puff then repeat steps 2-9 until you have given the number of puffs needed.

In an emergency you can give your child 10 single puffs of the blue inhaler using a spacer, over 5-7 minutes, while you get medical help and advice – this is called multi-dosing.
To use an aerochamber correctly:
- Get everything you need: inhaler, aerochamber.
- Shake the inhaler.
- Attach the inhaler to the aerochamber.
- Make sure your child is in a comfortable position – hold them if you need to.
- Put the mask over your child’s nose and mouth – press very gently to make a seal.
- Get your child to breathe in and out through the aerochamber.
- Press the inhaler once and,
- Count ten breaths (watch for a breath hold and you may need to put a hand on their abdomen to help you count the breaths).
- Take the inhaler away from the child’s face.
- Take the inhaler out of the aerochamber. Leave 30 seconds between each puff then repeat steps 2-9 until you have given the number of puffs needed.

In an emergency you can give your child 10 single puffs of the blue inhaler using a spacer, over 5-7 minutes, while you get medical help and advice – this is called multi-dosing.
To use a spacer correctly:
- Get everything you need: inhaler, spacer device.
- Shake the inhaler.
- Attach the inhaler to the spacer.
- Make sure your child is in a comfortable position – hold them if you need to.
- Put the mouthpiece between your child’s lips and teeth – make sure their tongue is not in the mouthpiece.
- Get your child to breathe in and out through the spacer.
- Press the inhaler once and,
- Count 5-10 normal breaths in and out – you should hear a clicking noise with each breath. (If you do not hear the clicking noise tilt the spacer up at the inhaler end – this will open the valve and help the child breathe in the medicine).
- Take the spacer away from the child’s face.
- Take the inhaler out of the spacer. Leave 30 seconds between each puff then repeat steps 2-9 until you have given the number of puffs needed.

Here are some triggers that people with asthma are sensitive to – which are your child’s triggers?
- colds/chest infections
- exercise/physical activity
- cigarette smoke
- cold weather
- changes in the weather
- laughing, crying or getting upset
- house dust (more later)
- animal fur/feathers
- pollens
- air pollution
Steroids for Asthma
What are steroids?
Steroids are chemicals made naturally by the body. They can also be made artificially as drugs. There are different types of steroids. Steroids made by the body to fight inflammation are called corticosteroids. If you have asthma, these corticosteroids help fight the inflammation in the airways. When you give your child their preventer medicine you are giving them the extra corticosteroids that they need.
Why do we use steroids in Asthma?
Steroids work by reducing the amount of inflammation, swelling and mucus in the airways. They are very effective for asthma if taken regularly.
How are they given?
There are three different ways that steroids can be given:
- inhaler – for daily preventive treatment. This gives a very low dose that goes straight to the lungs.
- tablets – short courses to cure an acute attack, or for use in very severe asthma. Prednisolone is the most common tablet.
- injection – for the very ill in hospital, or for children who have an upset tummy and can’t keep the tablets down.
What is the difference between inhaled steroids (preventer) and steroid tablets?
- The amount of steroid used in inhaled steroids (preventer) is much less than that used in steroid tablets. This is because the inhaled medicine goes straight to the lungs.
- One steroid tablet is at least 50 times stronger than a puff from a standard preventer inhaler.
- Because of this, side effects are not very common with inhaled steroids (preventer).
- Inhaled steroids (preventer) taken over a long period of time are safer for your child than lots of short courses of steroid tablets.
What about short courses of steroid tablets?
If your child’s asthma continues to get worse despite being on a preventer, then a short course of steroid tablets may be prescribed. Your GP or hospital doctor can prescribe steroid tablets.
A short course for just three to five days has few side effects, even with high doses. However, if your child needs steroid tablets often, the chance of side effects increases. That is why using preventer inhalers is better.

Steroids – side effects
Side effects are not very common with inhaled steroids (preventer). The medicine goes straight down to the airways where it is needed. Very little is taken into the rest of the body. Using a spacer helps even more of the medicine go exactly where it is needed.
Generally, low doses of inhaled steroids (400 micrograms daily or less) with occasional short courses of steroid tablets are enough to control asthma in most children. Side effects are more common in people with very severe asthma who have to take steroid tablets all the time.
To work out how many micrograms your child is taking, look at the label on your preventer medication. This tells you how many micrograms are given for each puff (actuation).
for example two puffs twice a day of Clenil Modulite 100 equals 400 micrograms daily.



What side effects are seen with steroids?
Side effects for children might be:
- mouth infections
- temporary slowing of growth
This is why we examine your child’s mouth and measure their height when we see them at the hospital clinic.
TIP: Using a spacer and brushing teeth or taking a drink after taking inhalers can help prevent mouth symptoms.
There is no evidence that steroids damage the lungs. However, asthma that is left untreated can lead to permanent lung damage.
NOTE: Steroids used for asthma are different from the body building (anabolic) steroids. Anabolic steroids do not reduce inflammation.
Growth
Will using inhaled steroids (preventer) stunt my child’s growth?
A great deal of research has been carried out on this.
- For children taking 400 micrograms or less a day no effect on growth has been found.
- There is some evidence that the growth of children who need over 400 micrograms a day may be slowed down in the shortterm. However, these children often have their growth spurt later and eventually reach their normal predicted adult height.
- Chronic untreated asthma in children will cause poor growth.
Adrenal glands
The adrenal gland produces the body’s own steroid, called cortisone. The body makes extra cortisone during illnesses like flu, tonsillitis, and gastro-enteritis.
When a child is taking high doses of steroids – either in tablet or inhaled form – the body produces less of its own steroid for a while.
When high doses of steroid medicines have been used and are cut down the body will slowly start making its own steroids again.
You must never suddenly stop giving high doses of steroid medicines that have been used for more than a few weeks. Your child’s body will not have enough of its own steroid to help fight illnesses like flu. It takes time for your body to make its own steroids again, so high doses of steroid medicines must always be cut down slowly.
Common questions about Asthma medicines
Do children get addicted to asthma medicines?
- No – children do not get addicted to preventer or reliever medicines. Children should always be allowed to use their reliever as soon as their asthma symptoms appear.
Do the inhaled asthma medicines lose effect if they are used too often or for too long?
- No – using inhaled steroids (preventer) every day does not mean that they become less effective. Your child’s body does not become so used to the medication that your child needs to take more and more of it.
How long does it take for the inhaled steroids (preventer) to start working?
- It can take a few weeks before you notice any improvement in your child’s asthma. It may be a few months before they feel the full effects of the inhaled steroids (preventer).
Can I change the amount of inhaled steroids (preventer) my child is getting depending on their symptoms?
- You should only change the amount of inhaled steroids (preventer) if you have agreed this with your doctor or nurse.
Is my child too young to start using inhaled steroids (preventer)?
- No. For children with asthma, inhaled steroids (preventer) are now standard treatment from infancy onwards.
Can I stop giving the inhaled steroids (preventer), but start again if the asthma symptoms return?
- Unfortunately, inhaled steroids (preventer) cannot cure asthma. For most children, inhaled steroids (preventer) have to be used every day without a break to get the full effect. If you feel your child’s symptoms are much better, discuss it with the doctor. It may be that the level of medication is just right and that is why your child has no symptoms. However, it may be possible to cut down the dose.
Will using inhaled steroids (preventer) stunt my child’s growth?
- See the section on Growth above.
My child only has symptoms in winter – do I need to use inhaled steroids (preventer) all of the time?
- For some children, asthma is only a problem at certain times of the year. It may be possible to give the inhaled steroids (preventer) only at that time.
My child only has symptoms with viral infections – do we really need inhaled steroids (preventer)?
- Some children who wheeze with viral infection (‘colds’) benefit from inhaled steroids (preventer), and some do not. Your doctor will check to see if the inhaled steroids (preventer) help your child. If your child is very allergic (eczema, food allergies) then steroids are more likely to be of benefit.
How long will my child need medication?
- This is very difficult to predict. Many children will need at least one or two years of treatment and sometimes much longer. The doctors will work with you to cut the medicines to the lowest dose and to stop them if possible.
Part 3 – Asthma at home – Peak flows
What is peak flow?
A peak flow meter measures how fast your child can breathe out.
If the airways are open the reading on the meter is high and if the airways are tight the reading is low.

Using a peak flow meter
How does my child use a Peak Flow Meter?
- Put indicator to zero
- Get child to stand up
- Ask them to take a deep breath and
- Seal lips around the mouthpiece
- Tell them to blow out as hard and as fast as they can – as though blowing out candles on a cake
- Write down the number
- Repeat this two more times
- The largest of the three numbers is your child’s best peak flow
Always do the peak flow readings BEFORE your child takes the asthma medicines.
How do I record my child’s peak flow?
The best way to do this is to keep a chart of their peak flow readings. We recommend measuring the peak flow first thing in the morning and last thing at night before taking any inhaled medicines.
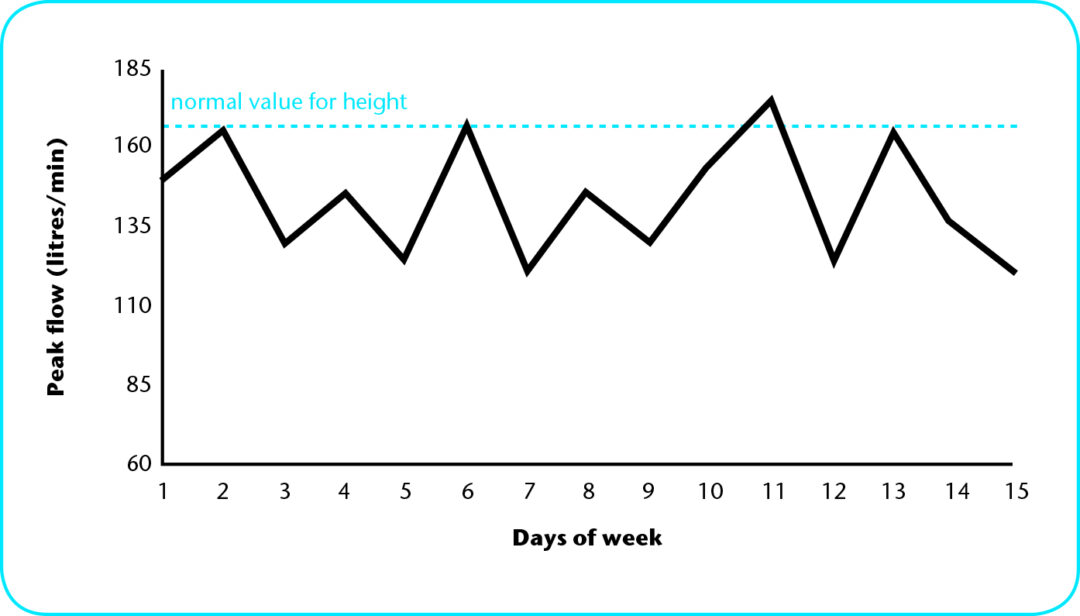
Below is an example of a peak flow chart that a child kept at home. The ‘up and down’ line happens when asthma is out of control.
How does a peak flow help me keep my child’s Asthma under control?
- Once you know your child’s best peak flow this will help you spot when your child’s asthma is getting out of control.
- When your child’s asthma is under control their peak flow readings will be fairly constant – the rate may vary up or down by about 8-10%.
- When your child’s asthma is getting out of control the peak flow will fall.
- If your child’s peak flow falls to 75% of their best they will usually have more symptoms and are likely to be wheezy. You should be using more reliever.
- If your child’s peak flow falls to 50% of their best they will be very wheezy/chesty. You need to use more reliever and contact your doctor. If you have steroids at home start giving these to your child.
These details can be added to your child’s Personalised Asthma Action Plan.
When can my child start using a peak flow meter?
Children can start doing peak flows from about five years of age. If they try when they are too young the readings are not always accurate.
What peak flow reading should my child have?
Peak flow will be different for every child.
Your child’s peak flow will vary depending on their height and their asthma diagnosis (if two children are the same height but one has mild asthma and the other has severe asthma the peak flow for the child with mild asthma is likely to be higher).
As your child grows their peak flow should get higher – it is important that you know what their best peak flow is (do not assume that the best peak flow they had 6 months ago is the same as it is now).
Avoiding Asthma triggers
There are triggers all around, and it is impossible to avoid all of them. You have no control over some, like the weather! However, here are some tips:
- Don’t smoke near your child, and your child should avoid smoky places.
- Avoid animals your child is definitely allergic to.
- In summer, avoid long grass.
- In the pollen season (summer or autumn) keep bedroom windows shut.
- Arrange for your child to play indoors on colder days.
- Remember to give them their reliever before any exercise.
- Ease your child gently into vigorous exercise.
The house dust mite
Children with allergic asthma are nearly always extra sensitive to the house dust mite. The house dust mite can be found in every home no matter how often you clean. The dust mite levels are highest in the living room and bedrooms.
1. Anti-house dust mite bed covers & sheets
There are new bedding sets (sheets, duvet covers and pillowcases) which are being recommended for asthma sufferers. Most dust in the bedroom is in the bed.
We think covers might help if your child is actually allergic to house dust mite.
However, these sets are expensive, and will not work unless you cover everything (pillow, duvet, mattress). If you do buy one, get a cover that the mattress fits right into. Just covering the top of the mattress is not good enough.

2. Avoiding house dust
Dust collects on furniture, carpets and soft toys. Here are some things that you can do to cut down dust in the bedroom:
- “damp dust” all surfaces in the bedroom every few days or so
- vacuum the mattress once a week
- change & wash all bed linen once a week (hot wash at over 60°C to kill the dust mites)
- wash soft toys or put in freezer monthly (in freezer for six hours, then vacuum the toy)
- washable blinds trap less dust than curtains
- laminate traps less dust than carpets
- avoid putting children with asthma in the lower bunk beds as dust constantly falls on top of the child

3. Anti-house dust mite sprays
You may also have heard about new chemical sprays which are now on sale. As yet these have not been very successful and they are still very expensive. Better to do the simple things first.
4. Does the make of vacuum cleaner matter?
There is some research being done in Britain right now looking at the different makes of vacuum cleaners. We do not know which is the best one to buy yet, so we cannot recommend one.
Part 4 – Coping with attacks
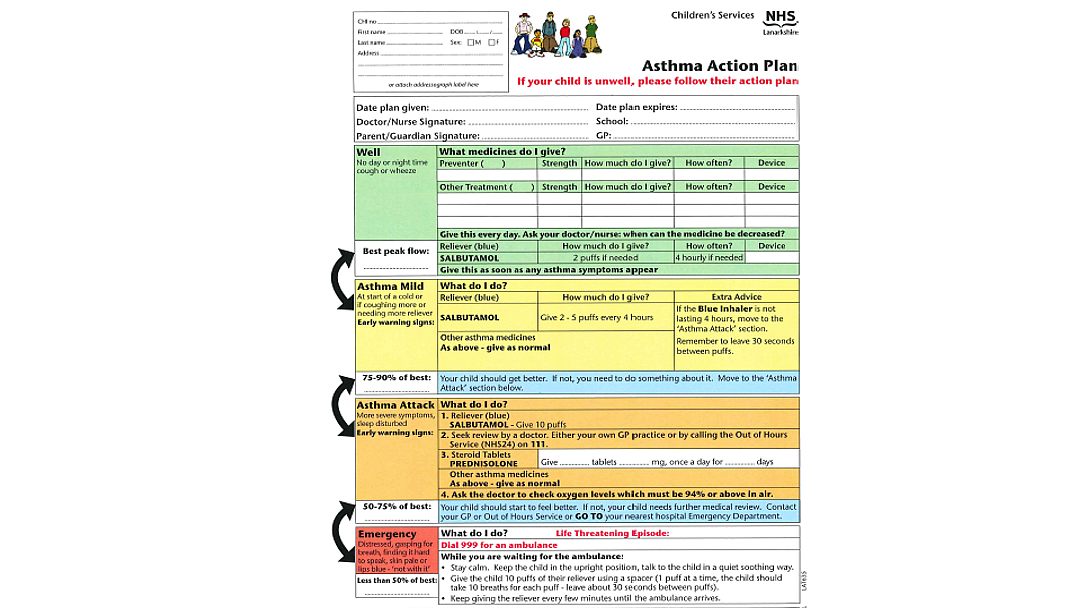
The next section shows you how to cope when your child’s asthma is getting worse. There are four action steps to take:
The 4 steps
- spotting asthma warning signs
- treating the warning signs quickly
- getting advice if things are not getting better
- knowing when to get emergency help
By acting quickly at home, you might stop the asthma attack getting very bad. You might even stop a hospital admission.
Read the next sections carefully. If there is anything that you still do not understand, ask the doctor or nurse looking after your child.

1. Spotting Asthma warning signs
Asthma attacks do not usually happen without warning. Most children have early warning signs. You might see these a day or two before the asthma flares up.
Can you see any of your child’s warning signs on this list? Add any others your child has.
You should start treating your child’s asthma as soon as you see the warning signs.
- Wheezy/noisy breathing
- Chronic cough, especially at night
- Difficulty breathing
- Chest starts to get tight or hurts
- Breathing faster than normal
- Getting out of breath easily
- Tired
- Itchy, watery eyes
- Itchy, scratchy or sore throat
- Stroking chin or throat
- Sneezing
- Headache
- Fever
- Very tearful
- Runny nose
- Change in face colour
- Dark circles under eyes
- Mood change
2. Treating the warning signs quickly
When you see the warning signs
As soon as you see your child’s warning signs start using their blue inhaler straight away – by acting quickly at home you might stop the asthma getting worse. You may even stop a hospital admission.
If symptoms are mild give up to five puffs of the blue inhaler using a spacer every four hours for a few days while symptoms last.
Breathing at night
People with asthma find it harder to breathe at night. In fact in the early hours of the morning everyone’s airways become a bit narrower. People without asthma don’t notice anything. People with asthma will find their breathing less easy at this time and may wake up.
Beware of Asthma signs at night
If your child’s asthma is getting out of control or an attack is coming on, an early sign may be waking at night with coughing or wheezing.


3. Getting advice if things are not getting better
The advice on this page is not to be used instead of seeing your family doctor or going to the hospital.
The tricky bit is knowing when to ask for help.
If you feel that your child’s symptoms are getting worse or you need to use the blue inhaler more often than every four hours, increase the blue inhaler to ten puffs every four hours AND contact your GP or NHS 24 – Telephone: 111 straight away for advice.
If you notice any of these, or if you are very worried about your child’s breathing you should call an ambulance straight away.
Remember – Don’t be afraid to make a fuss!
4. Knowing when to get emergency help
Your child will need emergency help if they are:
- Distressed
- Gasping for breath
- Unable to eat or drink
- Finding it hard to speak
- Looking pale or their lips going blue
- Quiet or drowsy
- ‘Not with it’
Going on holiday
With a bit of planning holidays are not a problem, even if you go abroad. Many parents tell us their child’s asthma gets better on their holidays.
- take your personalised asthma action plan*
- take enough asthma medicines with you
- take a spare inhaler in case you lose one
- take a written note of your asthma medicines
- ask your Family Doctor for some steroid tablets to take with you in case an asthma attack starts

* If you don’t have a personalised asthma action plan ask the nurses at the Hospital, or your Practice Nurse, to write out a plan to take with you.
Part 5 – General questions about Asthma
How can the doctor be sure my child has asthma?
- There is no definite test for asthma. Doctors can recognise the patterns of wheeze and cough seen in asthma. If your child is also helped by taking asthma medicines then they can be more sure it is asthma. It may take some time before the doctor is certain.
Will my child grow out of asthma?
- Not always – All children tend to improve around puberty. Surveys show that about half of children with asthma grow out of it when they are teenagers. For some, asthma comes back in their 20’s or 30’s.
Does air pollution cause asthma?
- There is no scientific evidence to prove that air pollution causes asthma. It does make asthma worse in people who already have it. Cigarette smoke is a very common culprit.
Should we try and re-home our pets?
- Trying to re-home your pets can be difficult and upsetting for the whole family. The best you can do is always keep them out of your child’s bedroom. Washing the animal weekly may help. If you are thinking about getting a pet, remember that an animal in the house may make your child’s asthma worse.
Should my child have the “Flu” vaccination?
- We think that children with asthma who need higher doses of the inhaled steroid (preventer), or have had an admission to hospital because of their asthma should get the vaccination. Ask your Consultant or family doctor if you are unsure. If your child is allergic to eggs, discuss vaccination with your doctor.
What is meant by Seasonal Asthma?
- Some children only get asthma symptoms at a particular time of year, such as the summer or autumn. This may be due to different pollens being in the air – grass in the summer or tree pollen in the autumn.
Can I try complementary medicines for my child’s Asthma? (Chinese, herbal, homeopathic, vitamin supplements, Buteyko method)
If you try a complementary medicine you should always continue giving your child their prescribed medication. Discuss any alternative treatments with the doctor.

Are complementary medicines safe?
Not always – some complementary medicines can have very serious side effects for people with asthma and should be avoided. For example, royal jelly can cause a serious allergic reaction. Natural remedies have not been researched as much as conventional medicines, so there is less information available about side effects.
Part 6 – Get the most from your Asthma team
The consultation
- Don’t be afraid to ask the doctor questions. If you don’t understand something or you want more information, just ask. The doctor is there to help you.
If you are upset about your child’s progress…
- Tell the doctor. They may think your child is doing well and see no reason to change things. Tell the doctor what is on your mind or what is happening. Your child may not get the treatment they need otherwise.
If you don’t understand what the doctor says…
- Ask questions. Doctors are busy and sometimes do not take enough time to explain things properly. They work with asthma every day. Things that seem simple to them may be complicated for you. If you say “I didn’t understand that”, you’ll remind them that not everyone is an asthma expert.
If you stop giving, forget, or increase the medicine…
- Don’t be afraid to tell the doctor this. Like you, they want to make sure that your child gets the minimum amount of medicine necessary to keep healthy. If you don’t tell the doctor, they may think your child’s asthma is better or worse than it really is. This could alter the dosage of steroids prescribed.
If you do not think you will stick to the medication the doctor has given you…
- Be honest with the doctor. If you have concerns about the medication, discuss them. You should be able to agree a plan with the doctor that you can stick to. Your child’s treatment should fit into your family’s routine.
If you have been told different things by different people about your child’s asthma…
- Tell the hospital doctor. They are experts in asthma. They have been specially trained and deal with it every day. The hospital doctor will help solve any conflicting advice that you have been given. But they can only do this if you ask.
If you are unsure how to give your child’s medication…
- Ask the doctor to show you how to use the inhaler/spacer.
- If it helps, take notes when talking to the doctor. Read them back to the doctor at the end, to make sure your notes are correct.
- When you think of questions between visits to the doctor, write them down so you remember them.
Personalised Asthma Action Plan
Please ask your nurse to give you a plan and fill it in with you. Every child’s plan will be different. Early and late warning signs help to take action earlier.
Going home with Asthma
Checklist for Parents
- Have you been told about the treatments your child has received?
- Have you discussed your asthma plan with nursing or medical staff?
- Do you have the medicines you need or a prescription for these?
- Do you know how and when to give these medicines?
- Have you been told about emergency asthma management at home?
- Have you been told about when to get help?

If you need this information in another language or format, please e-mail: