A B C Resuscitation of children aged one year and above
Information for patients
NHS Lanarkshire Neonatal Department
PIL.ABC10YR.11269.L
The need for resuscitation in children is very rare. However this leaflet provides guidance on the procedures you should follow in the event your child becomes unresponsive for any reason.
A is for Airway
As you approach the child, make sure there are no obvious dangers to yourself. Are there any indications the child is injured? If so, avoid any movement unless in a life threatening position.
Stimulate the child by placing a hand on the child’s head to stabilise it and tugging their arm or hair and shout “WAKE UP”. If you cannot wake the child shout for…
HELP!!!
If the child is unresponsive their airway must be opened immediately to prevent starvation of air. You should:
- Place the child on their back on a firm surface such as a table or the floor if necessary. If you find the child lying on the ground, do not move them, treat them where they are.
- Look in the child’s mouth for any obvious foreign bodies that you can remove but don’t blindly insert your fingers into their mouth as you may push a foreign body further in. If you think there is a foreign body use the choking manoeuvres described further on.
- Tilt their head back by putting one of your hands on their forehead and use the other to lift up their chin, be careful not to press on their neck while doing this. This is called a head tilt/chin lift manoeuvre and you should achieve a ‘sniffing’ position as shown in Picture 1 (head extended as if the child is sniffing something in the air).

B is for Breathing
With the airway open…
LOOK along the child’s chest (and stomach) for evidence of breathing
LISTEN for breathing noises from the child’s mouth
FEEL for their breath on your cheek
For no more than ten seconds.
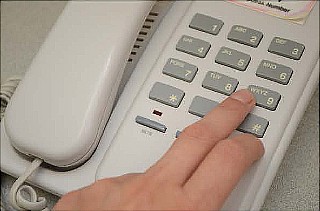
If the child is breathing normally, keep the airway open to maintain patency and ensure you, or someone dials 999 to summon emergency assistance from the ambulance service. You must tell them the child’s age, exact location, what happened to them and their current condition for example breathing but unresponsive.
Above all closely observe the breathing to make sure it doesn’t stop without you noticing.
If the child is not breathing normally or is just gasping, you must breathe for them…
- Pinch the child’s nostrils closed as demonstrated in Picture 2 below. Take a breath and place your mouth around the child’s mouth to create a seal and then blow slowly over approximately one second.

- At the same time watch for the chest rising from the corner of your eye.
- Remove your mouth and allow the chest to fall.
- Repeat this breathing procedure five times in total.
C is for Circulation
Take no more than 10 seconds to look for signs of life, such as swallowing, verbal noise, coughing and normal breathing.
If no signs of life, or you are at all unsure start chest compressions.
- Keep the child on a flat surface.
- Expose the child’s chest and place the heel of your hand on the centre of chest as shown in Picture 3, one finger breadth above the xiphisternum (base of breast bone where the ribs join together).
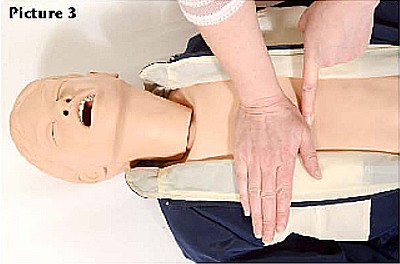
- Press down on the chest so it depresses by five centimetres (at least one third) of the chest depth. If you cannot press the chest down far enough using the heel of one hand, place your other hand on top of the first. You may need to do this for larger children.
Perform 30 compressions – rate: 100 -120 compressions per minute. You should aim for two compressions per second.
C is for Circulation (continued)
- After 30 compressions give the child two breaths as described before.
- If the ambulance is on the way continue until its arrival.
- If help has not been called give breaths and chest compressions for one minute before dialing 999. Alert the ambulance service and continue CPR. Do not interrupt the CPR unless the child wakes up or help takes over.
If your child has a known heart condition such as a congenital heart defect or arrhythmia (abnormal heart rhythm) alert the emergency services before starting chest compressions as a defibrillator may be needed.
Choking Manoeuvres (for children aged over one year)
Assess the child’s ability to cough
Cough – Effective
- crying – speaking
- loud cough
- able to breath before coughing
- fully alert
Reassure the child and encourage them to clear their airway by coughing.
Cough – Ineffective
- unable to vocalise/cry
- quiet/silent cough
- unable to breathe/struggling for breath
- going blue
- becoming unresponsive act quickly
SHOUT FOR HELP!!!
If the child is choking and unable to cough effectively, the following measures can be used to try to relieve the obstruction.
Choking Manoeuvres (continued)
Back Blows
- Support the child and hold them so their head is lower than the body as in Picture 4.

If your child has a mobility problem, roll them onto their side to enable you to access their back to administer the back blows or lean them forward while sitting in a chair.
- Support the child as you give up to five firm blows between the shoulder blades, using the heel of your hand as shown in Picture 5.

If the obstruction has not cleared after five back blows, attempt abdominal thrusts.
Abdominal Thrusts (sometimes called the Heimlich maneouvre)
- Stand behind the child and get them to lean forward if able. Identify a point on the child’s tummy half way between the bottom of the breast bone and their belly button as shown in Picture 6.
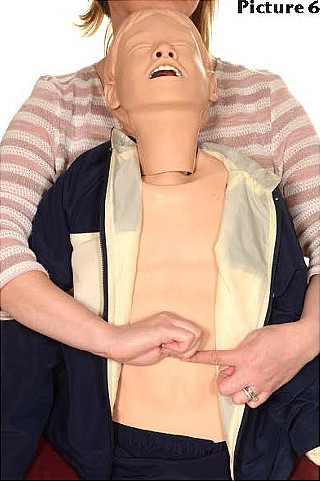
- Place a closed fist on this point and encircle the child’s waist with your arms. Grasp your own wrist.
- Pull sharply inwards and upwards, squeezing the child’s tummy.
- Repeat this up to five times if needed.
If the obstruction has still not cleared, repeat more back blows and alternate between up to five back blows followed by up to five abdominal thrusts until you succeed in clearing the child’s airway, or they become unconscious.
If the child becomes unresponsive after choking – get immediate help!! Dial 999. Ask someone else to do this for you if possible. Place them on a firm flat surface.
Check the mouth to see if you can see the foreign body, if you can, take one attempt to retrieve it. Do not try to retrieve an object if you cannot see it, you may push it further in!
Start CPR. Open the child’s airway into the ‘sniffing position’ as described earlier and Give five rescue breaths followed by 30 chest compressions. Continue CPR using 30 compressions to two breaths ratio until the child revives or help arrives.

Pub. date: November 2020
Review date: November 2022
Issue No: 04
Reference: PIL.ABC10YR.11269.L
20_17850
If you need this information in another language or format, please e-mail:





