Information for pregnant women who have a body mass index (BMI) of 30 and greater
Information for patients
NHS Lanarkshire Maternity Department
PIL.WHIBMI.69648.W
Introduction
Weight gain and changes to your body happen naturally as part of pregnancy. This can be due to the growth of your baby, the placenta and fluid surrounding your baby. However, if you are overweight at the start of your pregnancy, gaining more than the recommended amount of weight may put you and your baby at risk of pregnancy, labour and postnatal complications. Although it is recognised that increased weight can increase risk of complications many women who have a BMI of 30 and greater deliver their babies without any problems and with minimal intervention. Making healthy lifestyle changes will help reduce risks for both you and your baby.
At your booking visit your midwife will measure your height and weight using correct weight scales and stadiometer (height measuring tool). This will enable the midwife to discuss and plan your care appropriately for pregnancy, labour and after childbirth. You will not be routinely weighed again by your midwife until you reach 36 weeks pregnant. If your BMI is 30 and greater and you would like some additional support with making healthy lifestyle changes throughout your pregnancy, your midwife can refer you to the Healthy Lifestyle in Pregnancy Service. This is additional support from a midwife, physiotherapist and dietitian.
What is BMI?
BMI is a tool which uses height and weight to work out weight categories for adults over 20 years of age. BMI ranges are based on the effect that body weight has on health.
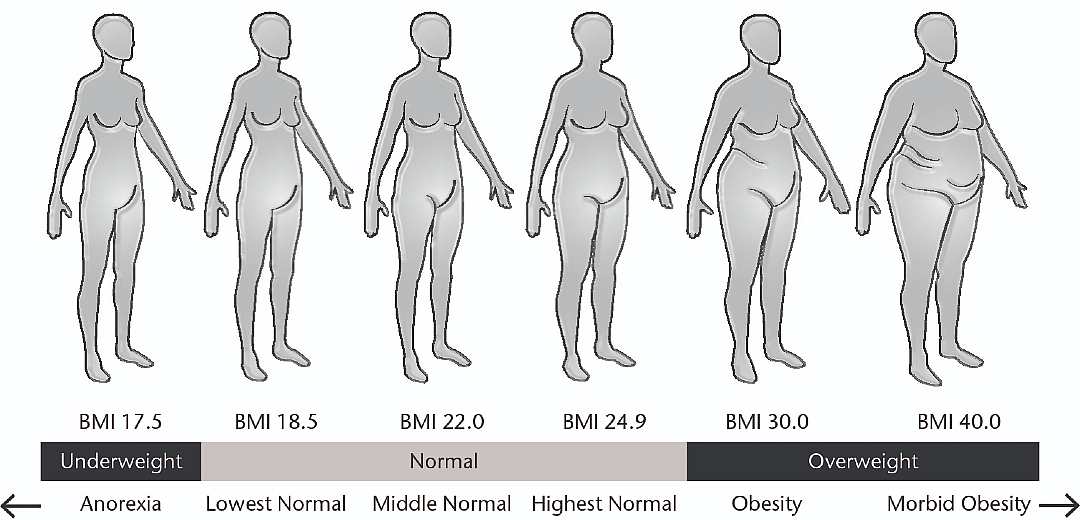
Two people could have the same BMI, however they could be very different in shape and fitness. Depending on which category you are in at your booking appointment, will determine recommended weight gain in your pregnancy.
BMI categories
| BMI kg/m2 | Definition | Recommended Weight Gain For Pregnancy |
| <18.5 | Underweight | 12.5 to 18kgs |
| 18.5-24.9 | Normal Range | 11.5 to 16kgs |
| 25-29.9 | Overweight | 7 to 11.5kgs |
| 30-34.9 | Obesity I | 5 to 9kgs |
| 35-39.9 | Obesity II | 5 to 9kgs |
| ≥ 40 | Obesity III | 5 to 9 kgs |
(SIGN, NICE, 2006)
How can I limit my weight gain during pregnancy?
You can limit weight gain by eating a healthy balanced diet and being active throughout your pregnancy. It is important to start with small achievable changes and these will have a positive impact on you, your baby and your family’s health, now and for the future.
Weight gain and changes to your body happen naturally as part of pregnancy, it is important you do not ‘eat for two’ and your midwife will advise you on weight gain. You will be weighed at booking and later during your pregnancy. If you have any concerns discuss this with your midwife.
You can manage your weight gain by:
- Choosing a healthier balanced diet, eating regular meals such as breakfast, lunch and dinner, cutting down on fatty or sugary foods and snacks.
- Try to eat at least 5 portions of fruit and vegetables per day.
- Drink fluids regularly at lest 6-8 cups or glasses (1.5 litres) daily. Choose water, diet or sugar-free drinks and limit caffeine intake to 200mgs/daily. (75mgs in a cup of tea 80-100mgs in a cup of coffee). Avoid alcohol completely.
- Choose foods rich in vitamins and minerals which are very important in pregnancy. Folic acid and foods rich in folate, such as oranges, green vegetables, fortified bread and breakfast cereals and brown rice reduce the risk of neural tube defects such as Spina Bifida. All pregnant women are advised to take a 400 microgram folic acid supplement which is contained in the free “Healthy Start” vitamins. Your midwife should give you regular monthly supplies throughout your pregnancy.
If your BMI is 30 or greater you will be advised to take a higher dose supplement of 5 milligrams. This can be given by your G.P. This supplement should be taken daily until 12 completed weeks of pregnancy and can be taken alongside your Healthy Start vitamins. - Your free Healthy Start vitamins also contain 10 micrograms of Vitamin D which is advised to be taken throughout pregnancy and whilst your baby is breastfeeding. We get Vitamin D from only a few foods such as oily fish. However we get it mostly from sunlight on our skin. Vitamin D is very important for the healthy growth of your baby’s bones. Ask your midwife for more Healthy Start vitamins when your stock is low.
- If your BMI is 30 or greater you will be offered referral to the Healthy Lifestyle in Pregnancy Service. You will receive support and guidance on eating healthily and managing weight from a Specialist Dietitian, Midwife and Physiotherapist.
- If you would like to know more about the service, call 07770 698955 or see the NHS Lanarkshire website for more information.
What are the risks for me if my BMI is 30 or greater?
- Infertility Problems
- Miscarriage
- Ultrasound scanning can be difficult and may not be as accurate in women living with overweight or obesity.
- Difficult to check growth and the position your baby is lying in.
- Difficult to monitor your baby’s heart beat during labour and it may be necessary to attach a small clip to your baby’s head to give a more accurate recording.
- You have a higher risk of anaesthetic problems:
-
- If you require an epidural for labour this can be more difficult to put in. It can take longer and despite a few attempts may not be possible to put in at all.
- There may be an increased incidence of complications such as headaches or nerve damage.
- Spinal or epidural anaesthesia (where you are awake) is preferred if you require caesarean section. These can be more difficult to put in or may not be possible to put in especially if you are in labour. This can cause problems such as headache or nerve damage.
- On some occasions it is necessary to have a general anaesthesia (where you are asleep) for caesarean section. If you have a high BMI it can be more difficult to put the tube in your wind pipe when you are asleep, resulting in low oxygen. It can also be difficult to help your breathing when you are asleep and this may cause low oxygen.
- If your BMI is 45 and greater your midwife will refer you to the Anaesthetic clinic where you will be seen around 28-34 weeks.
-
- Blood Clots (thrombosis) which can lead to serious complications and may be fatal. Post-natally you will be encouraged to get out of bed and move about as soon as you are able. You may be given an injection to prevent blood clots for 10 days. If your BMI is 40 and greater you will be given anti embolism stockings to wear which help reduce your risk of developing a blood clot.
- Impaired Glucose Tolerance
- Gestational diabetes, your midwife will check your urine sample at all antenatal visits. If your BMI is 30 or greater you will be offered a Glucose Tolerance Test (GTT) at 28weeks pregnant. This will be done to assess if you have developed this condition.
- High blood pressure and Pre-eclampsia. Your midwife will check your blood pressure at all antenatal visits.
- Complications in labour – such as shoulder dystocia (During delivery, the infant’s shoulder gets caught on the mother’s pubic bone) which may cause injury to your urinary and genital tract.
- Increased risk of Forceps/Caesarean section delivery.
- Wound Infections following caesarean section and increased risk of genital and urinary tract infections.
- Increased risk of maternal death
What are the risks for my baby if my BMI is 30 or greater?
- Prematurity which can cause serious problems for your baby
- Birth Defects such as Spina Bifida
- I.U.G.R (poor growth)
- Macrosomia (big baby)
- Metabolic problems such has hypoglycaemia (low blood sugar)
- Birth Injury such as nerve damage and possible bone fractures resulting from shoulder dystocia (see complications in labour above)
- Still birth (baby dying during pregnancy)
- Neonatal death (baby dying after delivery)
- Obesity in childhood and later life
Being active throughout my pregnancy
Being more active will help minimise your weight gain. Take part in activities such as, walking, housework, swimming, aquanatal classes, and gym exercises specifically for pregnancy. Always tell your gym instructor that you are pregnant. When exercising it is important not to overheat and you should drink water to keep hydrated. Also listen to your body, know your own limitation and don’t overdo it.
A BMI of 30 and greater can increase your risk of potential serious complications in pregnancy and childbirth. However, it is important to remember that many women will deliver their babies without any complications and minimal interventions.
Research has shown that making healthier lifestyle changes such as eating a balanced healthy diet and becoming more active during your pregnancy can have a positive impact on you, your baby and your family’s health now and for the future.
For more information on healthy diet and exercise refer to your pregnancy book ‘Ready Steady Baby‘. Information is also available through leaflets on electronic badger notes. Ask your midwife about local exercise groups available in your area. You can also check out the listed websites further down this page.
Further information
- Parent Club – Eat Better Feel Better
- www.food.gov.uk
- NHS Live Well – Healthy eating
- BDA Weight Wise website
- NL Leisure website
- SL Leisure and Culture
- BDA website – Pregnancy diet
Acknowledgement: Scottish Government healthier Scotland SNDRi How do I watch my weight during pregnancy? 2010

Pub. date: April 2022
Review date: April 2024
Issue No: 07
Reference: PIL.WHIBMI.69648.W
22_06241
If you need this information in another language or format, please e-mail:




