Postnatal Recovery Advice After Vaginal Delivery
Information for patients
NHS Lanarkshire Maternity Department
PIL.VAGDEL.21_22099.L
Pelvic Health Physiotherapy service
The NHS Lanarkshire Pelvic Health Physiotherapy service gives education and information to help you manage any pregnancy related musculoskeletal or pelvic floor problems.
It is very important to us that we give you the best evidence based information to help you make informed decisions about your care and promote healthy lifestyle choices.
We suggest you dip in and out of this leaflet during your postnatal journey to avoid feeling overwhelmed with the information.
Immediate management
In the first 24 hours after vaginal birth:
- Start your pelvic floor muscle execises.
- Drink 1.5 – 2 litres of fluid per day.
- Remember to empty your bladder every 3-4 hours (the sensation of wanting to pee may not return straightaway).
- Try to move around regularly.
- Avoid straining or holding your breath on movement.
Types of Vaginal Deliveries
A Vaginal delivery is any form of childbirth delivery that happens through the vagina. These include:
- Spontaneous Vaginal delivery
- Ventouse or Kiwi delivery
- Forceps Delivery
- Kielland’s Rotational Forceps delivery
Types of Perineal Trauma
- Perineum: The muscular area between the vaginal opening and the back passage
- Episiotomy: A cut made in the perineum and vaginal wall
- IAS: Internal anal sphincter (muscle that controls the back passage)
- EAS: External anal sphincter (muscle that controls the back passage)
- 1st degree: A tear involving a small area of the perineal skin
- 2nd degree: A tear involving the skin and muscle of the perineum
- 3a: A tear involving the perineum and less than 50% of the EAS
- 3b: A tear involving the perineum and more than 50% of the EAS
- 3c: A tear involving the perineum and both the EAS and IAS
- 4th Degree: A tear involving the perineum and EAS and the IAS and the lining of your bowel.
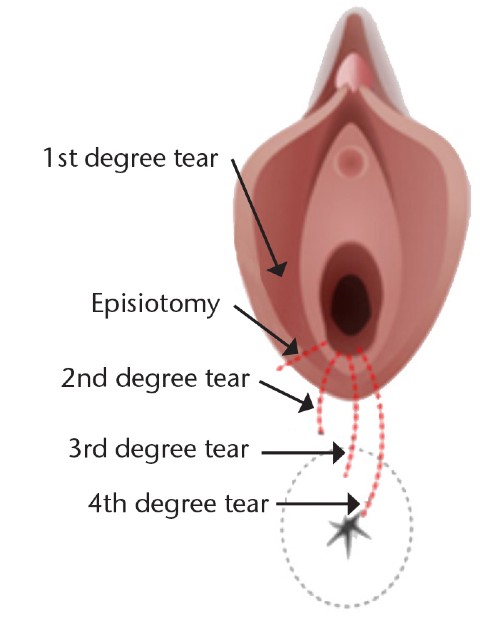
There are different degrees of perineal trauma that can happen during child birth. Around 90% of first time mothers who have a vaginal birth will have a graze, tear or an episiotomy. Grazes and 1st degree tears do not require stitches and heal quickly and naturally. 2nd degree tears and episiotomies are normally stitched by your Midwife, 3rd and 4th degree tears are repaired by a Doctor in theatre.
Perineal Care
Perineal tears are normally stitched to help with the healing of the tissues. Your stitches can take up to three months to dissolve. The perineum has a rich blood supply so it normally heals quickly. There are some simple things that you can do to help the healing process:
- Keep the area clean and dry by washing daily, pat dry and change sanitary pads regularly.
- You can bathe or shower but do not soak for long periods or use any soaps or perfumed products. Do not apply any creams or lotions to your stitches unless advised to do so by your doctor or midwife.
Speak to your GP or midwife if you notice any of the following: your stitches become painful or you have any strange smelling vaginal discharge, your wound is not healing, or your perineum is red in appearance or feels hard.
Managing swelling and pain
- It is important to rest little and often either on your back or side. This takes the pressure off your perineum, helping to reduce swelling and discomfort.
- Use ice packs wrapped in a clean, thin towel to help reduce swelling and pain. These can be placed on the tender area for up to 10 minutes. Make sure you do not put ice directly onto the skin.
- To make sitting more comfortable, sit on a pillow or place a small rolled up towel under each thigh so that your perineum is not in contact with the chair. NOTE: Ring cushions are not advised as they can increase swelling around the perineum.
- Exercising your pelvic floor muscles will encourage better circulation, healing and reducing swelling.
- Use pain relief medication regularly as suggested by your doctor or midwife.
Bladder Care
- You should pass urine in the first 4 hours after your delivery or once your catheter has been taken out. If you are having difficulty passing urine or not feeling the urge to empty your bladder, please speak to the midwife in charge of your care.
- If you are having any leakage of urine or not getting to the toilet in time, please speak to the midwife in charge of your care.
- Aim to drink 1.5 – 2 litres of fluid every day, especially if you are breastfeeding.
- Avoiding caffeinated drinks e.g coffee, tea, Cola, Irn-bru can help to reduce any bladder irritation.
- It is important not to pass urine too often throughout the day. You should empty your bladder every 3-4 hours.
If you are having difficulty emptying your bladder when you are discharged home, please contact Maternity Triage on 01698 366210.
Bowel Care
It is common to feel nervous about opening your bowels after delivery but do not worry, your stitches will not be affected.
- Do not ignore the urge to empty your bowels.
- To make emptying your bowels feel more comfortable, wrap your hand in some toilet paper or use a maternity pad and apply gentle pressure over your stitches.
- Try to avoid constipation by eating a healthy diet with high fibre foods such as: porridge, wholemeal bread, vegetables, beans, seeds and nuts. You will find more advice and a link to the British Dietetics Association on page 19.
- Ensure you have a good fluid intake of 1.5 – 2 litres per day.
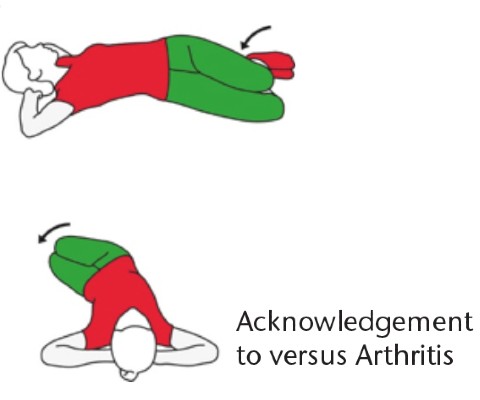
- Avoid straining to empty your bowels by sitting in the position in the picture below, relax your tummy muscles, take deep breaths into your low tummy and take time to empty your bowels.

Acknowledgment to Crohn’s UK for image
- Keep back straight
- Spread feet wide
- Lean forward
- Put elbows on knee
- Keep knees higher than hips
Circulation
It is important to get out of bed and move around. Try this little and often, soon after delivery. This helps to promote good circulation around your body. However, if you have been advised by your midwife or doctor not to get up, please follow their instructions about when you should do so.
- It is normal to have swollen ankles and feet after delivery. Raise your legs above your heart to encourage the fluid to drain away from your feet.
- Circle your ankles 20 times every hour whilst resting to help to reduce the swelling.
- If you notice any redness, swelling or pain around the back of your calf – please contact triage on 01698 366210.
Advice for home
When you get home after your hospital stay, your full attention will be on caring for your baby. It is important not to forget about the important advice in this booklet during your day to day activities.
- Try not to lift heavy items around the house for the first few weeks.
- Complete household tasks steadily so you do not tire yourself out
- When you’re getting out of bed roll onto your side first then take your legs over the edge of the bed and use your arms to push yourself up to sitting.
- When you are feeding your baby make sure your back is well supported and you are sitting or lying in a comfortable position.
- Try to change the side that you feed and carry your baby on, especially as they get bigger.
Pelvic Floor Muscle Exercises
What are the pelvic floor muscles?
The pelvic floor muscles are a large group of muscles that support your bladder, womb and bowel. They provide strength and structure to your vaginal walls. Your pelvic floor muscles also help to control passing urine and opening your bowels.
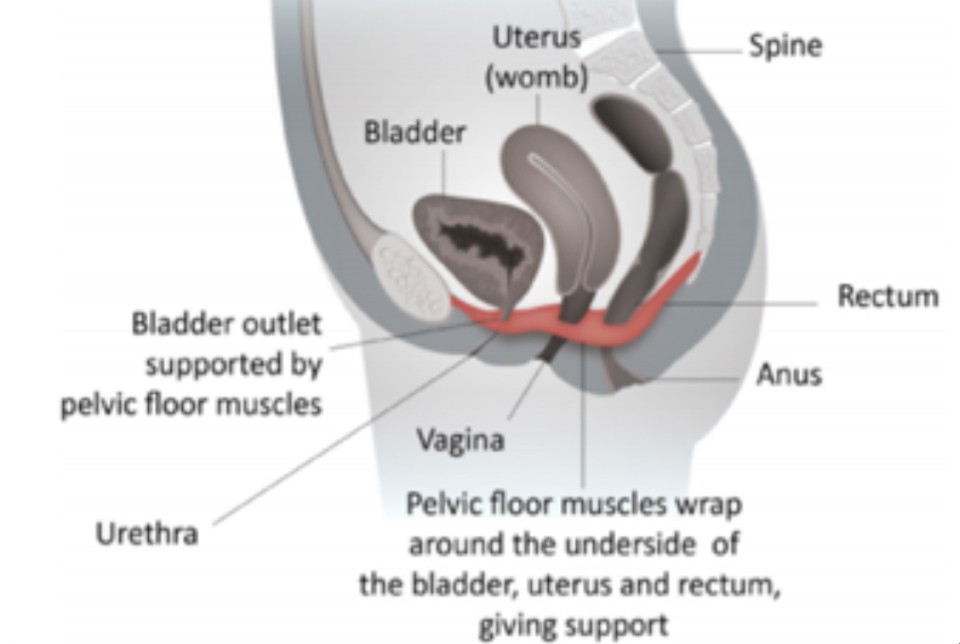
Why do I need to strengthen my pelvic floor muscles?
Pregnancy puts a lot of pressure on your pelvic floor muscles and it is normal for the pelvic floor muscles to stretch during a vaginal birth. Your muscles may be weaker and you may feel more pressure vaginally, so it is very important to strengthen your pelvic floor muscles soon after you have had your baby.
By doing your pelvic floor exercises you can avoid having symptoms such as leaking urine when laughing, coughing, sneezing and symptoms of vaginal heaviness.
When can I start my Pelvic floor exercises after delivery?
These exercises should be started as soon as your catheter has been removed (if you have had one) or when you have passed urine normally and your pain is under control.
How do I strengthen my pelvic floor muscles:
Start these exercises lying on your back or side. Then progress to doing them in sitting or standing.
- Step 1: Tighten the muscles around your back passage as though you are holding in wind (without squeezing your buttocks).
- Step 2: At the same time as your back passage squeeze, zip forwards to lift the muscles around the opening to your vagina, think about stopping yourself from passing urine.
- Step 3: Lift and squeeze your pelvic floor muscles quickly 10 times.
- Step 4: Lift and squeeze your pelvic floor muscles for up to 10 seconds 10 times. Relax for 4 seconds between squeeze.
- Step 5: Try and complete these exercises when you are feeding your baby or three to four times every day.
Note: Do not hold your breath when completing these exercises
Reminder: Your pelvic floor muscle exercises are for life and can help to prevent you having bladder, bowel or prolapse symptoms in the future.
You can download the blue NHS pelvic floor app called ‘Squeezy App for Women’ to help remind and guide you through the progression of these exercises.
‘The Knack’
Before you cough, sneeze or lift your baby you should try to tighten your pelvic floor muscles. This can help to support your bladder and reduce the risk of bladder leakage.
Abdominal Muscles
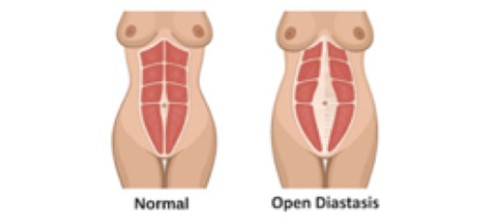
What is Diastasis Recti?
During your pregnancy your abdominal (tummy) muscles stretch as your baby grows. This causes the stretch of the abdominal muscles and the fibrous structure that runs down the middle of the tummy, and is called Diastasis Recti.
- This happens to every woman when they reach 35 weeks of pregnancy, but it can appear from 25 weeks.
- This can be seen earlier in women carrying twins or those who have had a previous diastasis.
- It is estimated that approximately 3 in 10 women have an ongoing diastasis. The recovery can take between 9 weeks to 2 years after delivery, this is normal.
- To help the abdominal (tummy) muscles recover, we recommend you complete regular low level, core exercises.
We would advise that you start with Postnatal Pilates around 4 weeks after delivery.
Different variations of Diastasis Recti
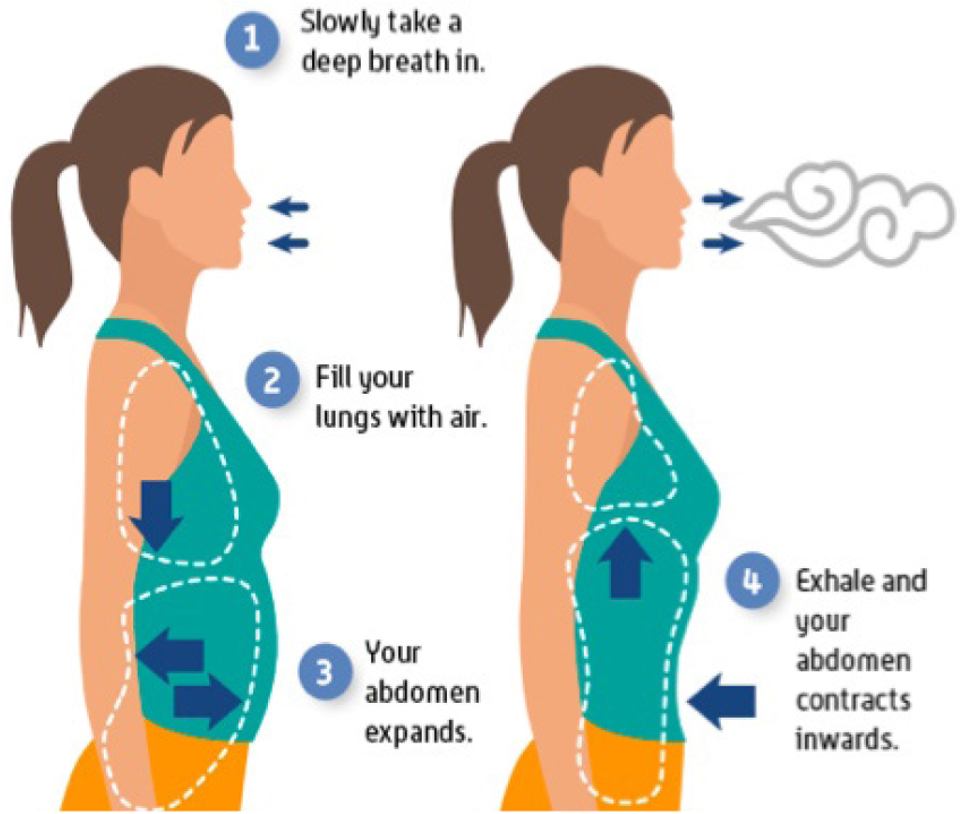
Exercise 1: Basic abdominal contraction
Sitting or standing:
- Breath into your stomach by relaxing your tummy muscles
- Breath out and draw your lower tummy muscles backwards to your spine.
- When completing this exercise make sure you keep your shoulders, rib cage and jaw relaxed.
- Repeat 5 times.
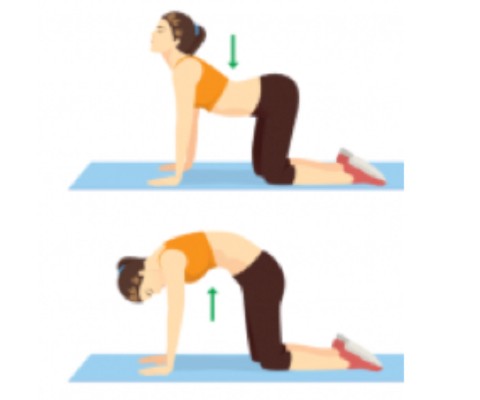
Exercise 2: Pelvic Tilts
This exercise can be done lying down with your knees bent, lying on your side, sitting down or on your hands and knees.
- Complete the basic abdominal contraction described above.
- Breathe in and push your tail bone towards the floor and arch your back.
- Breathe out and roll off your tail bone to flatten your back against the floor. Hold this position for a few normal relaxed breaths.
- Repeat this 5-10 times.

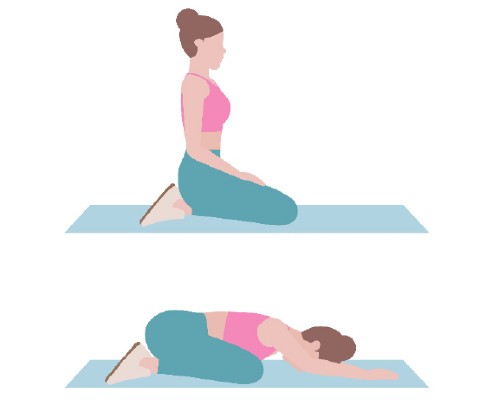
Lower Back Pain and Shoulder Pain:
Due to repetitive movements with your baby (e.g changing nappies, feeding and bending over) the upper body, shoulders and lower back can get stiff and painful. We would advise that you try some of these exercises once a day to avoid having any stiffness in these areas.
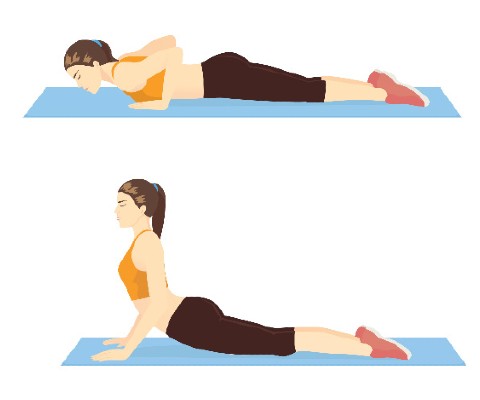
These exercises combined with your pelvic floor muscle exercises help you to have strong core muscles around your pelvis. This will make it easier to move forward with your postnatal journey and begin your return to exercise.

Returning to Sex (6 weeks after delivery)
When is it safe to have sex again?
Many woman worry about having sex after childbirth, particularly if you have had stitches. Once bleeding has stopped and your stitches have healed, you can have sex again when it feels right for you and your partner. There are some things that might help:
- Use a vaginal lubricant
- Find a position that is comfortable for you. This will make penetration more comfortable.
- Perineal massage – once your stitches have healed some gentle massage over your scar can make sex more comfortable.
It is normal not to feel ready to have sex for a few months after delivery. If you have tried to have sex a few times and continue to have pain, you should contact your GP or NHS Pelvic Health Physiotherapist for advice.
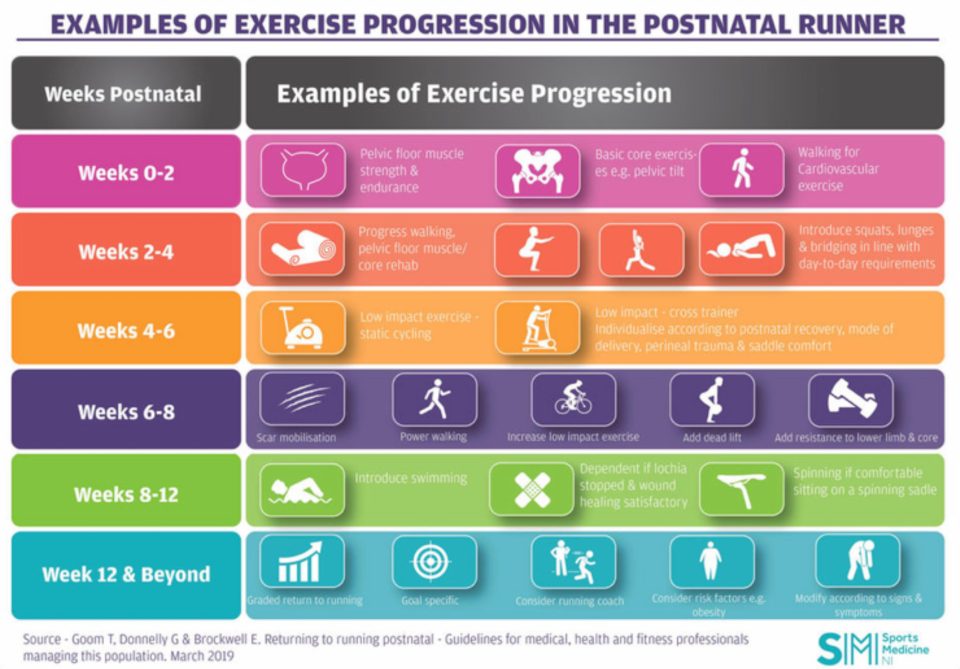
How long should I wait before going back to exercise?
It is suggested that you always build up slowly over time and listen to your body by being aware of any symptoms that develop during or after exercise. The ‘Return to Exercise Guideline’ on page 16 is a good programme to follow to allow you to return to exercise safely.
|
Myth |
Fact |
|
“My core will always be weaker after childbirth.” |
If you do the right exercises your core can be just as strong as it was before pregnancy. |
|
“I can return to all exercise after my 6 week check from the GP.” |
It is important to progress your exercise slowly like described on page 16 in the return to exercise guideline. |
|
“Incontinence after childbirth is normal.” |
Incontinence is very common after childbirth but never normal. It is advised that you follow all the fluid diet and pelvic floor advice in this booklet to reduce the risk of having pelvic floor dysfunction. |
Am I ready to return to impact based exercise? (12 weeks after delivery)
You do not need to work exactly to the timeframe shown on page 16, but it is advised that you do complete the exercises in this order to prepare your body for impact based activity such as running, jumping and resistance training.
| Exercises | Leakage | No leakage |
| Lunges (x 10 for each leg) | ||
| Single leg balance (30 sec R+L) | ||
| Forward bounds (x 10) | ||
| Jog on spot (1 min) |
Do I need Pelvic Floor Physiotherapy? (12 weeks after delivery)
If you have tried all the advice in this booklet and you are still having issues with your pelvic floor, then answer these questions to see if you need Pelvic Floor Physiotherapy input.
| Yes | No | |
| 1a: Do you usually have leakage from your bladder when coughing, sneezing or laughing? | ||
| 1b: Do you usually have leakage from your back passage/bowel when coughing, sneezing or laughing? | ||
| 2: Do you have a sudden need to pass urine with little or no time to get to the toilet? | ||
| 3: Do you have pain during sex? | ||
| 4: Do you have a heaviness or dragging feeling in your vagina? | ||
| 5: Do you have worries about your abdominal (tummy) muscles? | ||
| 6: Do you have constant back or pelvic pain that affects your day to day life? |
If you answer yes to any of the above questions 3-6 months after your delivery, please contact our NHS Pelvic Health Physiotherapy service. If it has been over 6 months since you have delivered your baby, please speak with your GP for a referral to the right service.
Glossary
- Abdominal Muscles/Core: The tummy muscles.
- Antenatal: The period of time that you are pregnant.
- Bladder: A muscular sac that holds urine.
- Catheter: A flexible tube inserted into the bladder to remove urine.
- Circulation: The movement of blood around your body.
- Constipation: A condition in which there is a difficulty in emptying your bowels due to hardened stool.
- Linea Alba: A fibrous tissue that runs down the middle of your abdominal muscles.
- Mucosa: The inner lining of your vagina or bowel.
- Musculoskeletal: The muscles and skeleton.
- Perineal Massage: Massage of the skin between the vagina and the back passage.
- Postnatal: The period of time after you deliver your baby
- Prolapse: When your bladder, womb or bowel move from their normal position and bulge down into the vagina.
- Straining: To make a great effort, push or hold your breath on a movement
- Urine: The fluid stored in your bladder and is emptied when you go to the toilet.
- Uterus/Womb: The organ in which your baby grows before you give birth.
- Vaginal Lubrication: A vaginal discharge to allow smooth movement.

Publication date: November 2021
Review date: November 2023
Issue Number: 01b
Reference: PIL.VAGDEL.21_22099.L
22_03843
If you need this information in another language or format, please e-mail:





