Neurological Condition - Moving Forward

Produced in conjunction with GCU Physiotherapy
Introduction
Keeping active is important to everyone, particularly people living with neurological conditions.
Being active helps to reduce issues such as muscle, joint, bowel and breathing problems.
This webpage outlines essential information, exercises and support to help you, or someone you care for, in ‘Moving Forward with a Neurological Condition’.
The Team
- Physiotherapists
- Occupational Therapists
- Orthotists
- Dietitians
- Speech and Language Therapists
Muscle Tone Management
What is Muscle Tone?
Muscle tone is the amount of tension in a muscle when it is not moving. It can be high, low or normal and affects how we move
Altered muscle tone is common in people with neurological conditions.
Uncontrolled movements are common too and can be known as Dystonia.
Why Does it Matter?
Good muscle tone helps to:
- Reduce pain
- Improves your posture
- Helps activities of daily living
See the dropdowns below for ideas to manage muscle tone problems.
Physical Treatment
- Splinting and Casting
- Postural Care
- Passive or active exercise can help
- The multidisciplinary rehabilitation team may include: Physiotherapists, Orthotists, Occupational Therapists, Speech and Language Therapists and Dietitians.
Medical Treatment
- Medical treatments for muscle tone work to relax and reduce your muscle tone.
- Treatments such as Botulinum toxin (Botox) can be injected into your muscle to relax it
- Oral Medication (tablets that you swallow) such as Baclofen may make all of your muscles more relaxed
- Medication and injections only work if you are also having physiotherapy
- For more information go to the NHS Inform website
Splinting and Casting
- Splinting and serial casting can be used to manage changes in your muscle tone and improve the range of motion and movement in your joints.
- Splints help to stretch your muscles and keep your joint in a good position.
- For more information go to the NHS Inform website
Postural Care
What it is?
Postural care aims to improve your body’s position when you are sitting, lying down or standing. It is important that you think of your postural care throughout the day and night; this is also known as 24-hour postural care.
Poor positioning and posture can lead to muscle and joint problems such as:
- Increased muscle tone (a ‘tight’ feeling in your muscle)
- Reduced muscle strength (your muscles feeling weak)
- Reduced voluntary movement (a ‘stiff’ feeling)
- Not being able to change positions easily
Postural care can be broken up into lying, sitting and standing postural care.
Why Does Postural Care Matter?
There are several benefits that you will get from having good postural care:
- Relief/prevention of pain
- Reduced risk of scoliosis
- Improved circulation
- Prevention/reduction of pressure sores:
- Can take part in activity more easily
- Pamis postural care video
Lying Down Postural Care
- The average person spends around half of a 24-hour period in a lying down position. This is around 3000 hours per year.
- Good night-time positioning is important as we spend a lot of time lying down
- When we are lying down our bodies are in contact with a bigger area of the bed, sofa etc – we call this the ‘body base of support’. This means there is less gravity working on our muscles and they are more relaxed. See the muscle tone section for more information
- When your body is relaxed, your posture can be corrected and improved
- Your night-time sleeping position can be improved using cushions, rolls, wedges and specialist sleep equipment that your physiotherapist can tell you about.
Sitting Postural Care
- Sitting may be the only alternative to lying down for you
- It is important that you sit in an upright position, with a straight back and shoulders, facing the front
- Seating that can be adjusted to fit you (‘supportive seating’) helps to give you the best posture
- This type of supportive seating also give you a good position for safe eating and drinking and reduces the risk of something ‘going down the wrong way’
Standing Postural Care
If you cannot stand unaided you could use a walking aid or standing frame.
Ask for advice from a physiotherapist.
Standing can:
- Improve your breathing
- Improve your circulation
- Stretch your muscles and joints
- Keep your bones strong
- Help your digestive, bladder and bowel functions
Types of Movement
What are they and how do they help?
Passive Movements these are exercises and movements that someone else will do on your muscles and joints if you are unable to move yourself.
- Passive movements can help you to maintain movement and reduce joint stiffness
- Passive movements help reduce any discomfort or pain you might have
Active-assisted Movements these are exercises and movements that you do yourself with some help from another person or a mechanical aid such as a weight or band.
- These may be a progression towards active movements or where greater user participation is possible.
Active Movements are carried out by yourself
- Active movements help keep your muscles strong and maintain movement.
Short Instructional Videos
Please read the list of safety precautions before continuing with these activities.
Passive Movement videos and booklet:
Safety Precautions
Precautions before starting:
- Wear loose clothing that does not restrict movement.
- Don’t let your helper force any part of your body. If pain occurs, stop. Check with your physiotherapist before trying that movement again. The shoulder joint can be particularly prone to trauma if not moved correctly. If any discomfort occurs, ask to go back to a movement that’s easier.
- It’s important to distinguish between pain and the feeling of stretch. Talk to your helper when they are moving your limbs. A feeling like stretching a tight elastic band is okay; pain is not.
- Remember to breathe evenly and relax throughout each movement. There can be a tendency to hold the breath during movement.
- Experiment with times of day. Some people find morning best; some find it helpful to break exercise sessions into two parts: one in the morning and the other in the afternoon or evening.
Some safety instructions for the helper:
- If the person you are helping is in an electric or hospital bed, raise the height of the bed to a comfortable level so that you are not putting strain on your back.
- If the person is in a normal bed, sit or kneel in a comfortable position.
- Don’t try to “fight” a spasm or tight muscle. This could result in injury to both of you. Move slowly, to allow tight muscles to relax and spasms to reduce. Sometimes holding a position will allow the spasms to pass. Moving quickly can increase stiffness. (For more information on this, see page 14)
- You may be able to incorporate some of these movements if you are washing or dressing the person.
- Keep communication open – look at and listen to the person you are helping.
- Hold each stretch for several seconds. Then gently return to the starting position. Repeat each exercise 2-3 times.
Moving Functionally (Moving Around)
“Functional Moving” is simply moving safely and independently. For people with neurological conditions, moving functionally can be difficult due to the changes in their muscle tone, strength and coordination. Moving around improves your well-being and can reduce your risk of falls through developing better balance.
Who can help you to live and move functionally?
Physiotherapists
Can assess and suggest ways to carry out your tasks and activities, which can help you to improve your muscle use.
Occupational therapists
Can also assess your ability and suggest activities or equipment that will help you to maximise your ability to carry out activities of daily living. Activities of daily living include tasks like feeding ourselves, bathing and showering, going to the toilet, dressing, working, and doing housework.
Yourself
You can try to stay active with different activities which will help your movement and functional ability.
Functional Movement Skills
Physiotherapists and Occupational therapists can help you achieve these functional tasks.
- Rolling / bed mobility
- Transfers from chair to bed
- On/off toilet
- On/off floor
- Sit to stand
- Sitting balance
- Standing balance
- Improve your walking pattern
Physical Activities
Physiotherapists and Occupational Therapists can help you with an assessment and then can offer advice and suggest activities that will help you to participate in more activities.
- Bowling
- Yoga
- At home exercises
- Sports
Creative and Social Activities
Creative and social activities can include things like:
- Baking
- Painting
- Playing
- Drawing
- Word search
- Crossword puzzle
- Reading
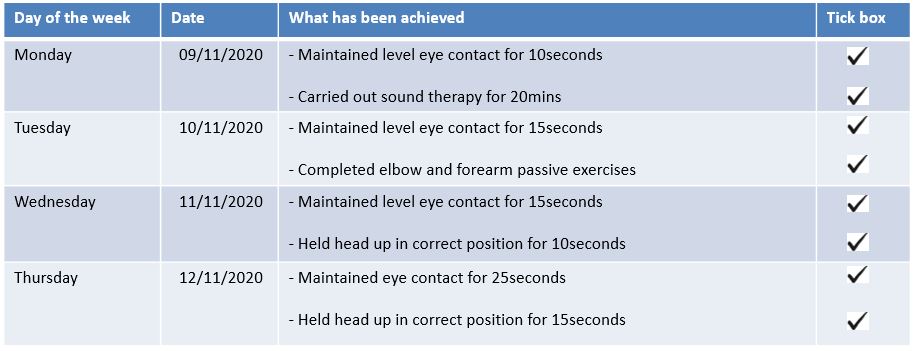
Achievement Chart
Achievement charts are a great way for you to keep track of your daily achievements. These can be as small as holding level eye contact for longer than 10seconds or something bigger as being able to achieve sitting balance for longer than 3minutes, depending on what you want to work on to achieve your goals. A simple way to keeping track would be to measure each activity with time or increasing the repetitions. Here is an example below:
Selected Neurological Conditions
- Angelman Syndrome
- Brain Injury
- Cerebral Palsy (CP)
- Huntington’s Disease
- Motor Neurone Disease (MND)
- Multiple Sclerosis (MS)
- Parkinson’s Disease (PD)
- Rett’s Syndrome
- Stroke
Online Activities
- Scottish Ballet – Dance for Parkinson’s
- The Brain Charity – Free Online Activities
- Exercise classes for adults with Cerebral Palsy
- Scottish Disability Sport
- Riding for the disabled association
- Inclusive gyms
- Neuro Therapy Centre – Home Exercise Classes
- Fitness training for children, adolescents and adults with Cerebral Palsy
- Parkinson’s UK YouTube Channel
- CP Sport
- Zoom Pilates classes
- PAMIS – Leisure Activities
Guidelines
- NHS Physical activity guidelines – PDRU
- Postural care and people with learning disabilities: guidance
- Spasticity in under 19s: management
- Cerebral Palsy in adults
- Care and support of people growing older with learning disabilities
- Learning disabilities and behaviour that challenges: service design and delivery
- Urinary incontinence in neurological disease: assessment and management
- MS trust – Posture and MS
- NES Postural Care – protection of body shape
- NES – Postural Care during COVID-19
Your Feedback – comments, concerns and complaints
NHS Lanarkshire is committed to improving the service it provides to patients and their families. We therefore want to hear from you about your experience. If you would like to tell us about this please visit our feedback page.

